Symptoms and treatment of pericarditis in adults
Author Ольга Кияница
2019-03-03
Pericarditis can be considered as a separately developing disease or as a syndrome if its cause of occurrence is associated with another disorder. It can occur both in adults and in childhood, but is more often defined in men aged 20 to 50 years.
Pericarditis can be constrictive, acute and recurrent, and it develops for various reasons, from traumatic injury to infection.
During the examination of the patient the diagnosis can be made already during an objective examination. Nevertheless, laboratory and instrumental methods of examination (ECG, echoCG, X-ray) are used to clarify the diagnostic conclusion.
Video: Pericarditis - Causes, Symptoms, Diagnosis, Treatment, Pathology
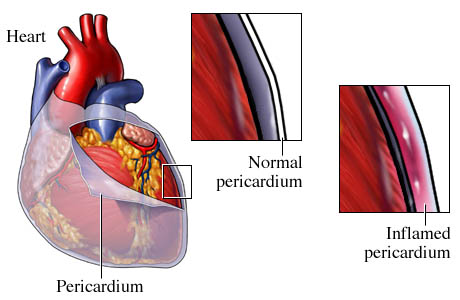
Description of pericarditis
Pericarditis is an inflammation of the pericardium, the so-called pericardial sac or serous membrane surrounding the heart. Pericardium is necessary to protect the heart from mechanical damage and reduce friction between the heart and surrounding organs.
Pericarditis may be accompanied by effusion, which is the accumulation of fluid in the pericardial pouch. If a large amount of fluid builds up in the pericardium, it can squeeze or squeeze the heart, then heart tamponade is said.
Heart tamponade is a serious disease that can be life-threatening if not recognized and not treated promptly.

Causes of pericarditis
Pericarditis has many causes, including the following:
- Infectious lesion . Any infectious organism can cause the development of inflammation in the pericardium. Most cases are caused by a viral infection or an unknown organism.
- Irradiation . Prior chest irradiation is an important cause of pericardial disease. Most cases are secondary to radiotherapy of malignant tumors, especially in breast cancer, lung cancer or lymphoma.
- T is a damage . Trauma to the chest can be blunt, as when hitting the steering wheel, or acute, as if a bullet or knife wound. Invasive cardiac procedures and rarely cardiopulmonary resuscitation (CPR) can cause cardiac injury, which is further complicated by pericarditis. In myocardial infarction (heart attack), the heart muscle can also be injured due to the lack of oxygen, against the background of which pericarditis develops.
- Medicines and toxic substances . A number of drugs can cause pericarditis.
- Metabolic disorders . The main cause of metabolic pericarditis is renal failure.
- Cancer neoplasms . Pericardial inflammation can develop when the cancer metastasizes (spreads) in the heart, most often from the breast, lung, or Hodgkin's lymphoma.
- Rheumatic diseases . Systemic lupus erythematosus, rheumatoid arthritis, systemic sclerosis, and mixed connective tissue diseases are the most common rheumatic causes of pericarditis. Other possible causes include systemic vasculitis and auto-inflammatory diseases (for example, familial Mediterranean fever).
- Gastrointestinal pathological conditions . Patients with inflammatory bowel disease (ulcerative colitis or Crohn's disease) may experience pericarditis.
Another disease can develop for no apparent reason, and then they talk about idiopathic pericarditis. In many cases it is not possible to determine the cause of the disease pericardium. It is also not always necessary to establish the cause, especially if the condition improves with empirical anti-inflammatory treatment (for example, by taking aspirin, ibuprofen).
Symptoms and diagnosis of pericarditis
The most common symptom of acute pericarditis is chest pain, which is usually worse with a deep breath. This pleural chest pain begins suddenly, is often acute and is felt in front of the chest or to the left of the midline.
There may also be an instant chest pain of a dull character, like a heart attack. The pain may decrease in a sitting position and spread around the left shoulder towards the upper back. Some people with pericarditis and pericardial effusion develop fever.
General characteristics of chest pain in pericarditis in adults (in 95% of cases):
1. Time: it starts suddenly, lasts from several hours to several days.
2. Character: manifests as acute pleural chest pain.
3. Localization: chest pain or left-sided chest pain
4. Irradiation:
a. Trapezoid ridge due to irritation of the left phrenic nerve (very specific for pericarditis).
b. Neck, jaw or shoulder (similar to myocardial infarction).
5. Modifying factors:
a. Not relieved after taking nitroglycerin.
b. Chest pain increases when swallowing, inhaling, coughing.
c. The condition worsens in the supine position.
d. It becomes better in a sitting position, leaning forward.
Acute myocardial infarction may also be present in pericarditis, therefore, due to symptoms alone, it is difficult to diagnose pericardial inflammation.
Examination of the patient
Pericarditis is diagnosed on the basis of physical examination, laboratory and visual research.
- Physical examination . During a medical examination, the heart will be heard with a stethoscope. In addition, people with pericarditis often have abnormal heart sounds, called pericardial friction. This sound is created when inflamed pericardial membranes (visceral and parietal) rub against each other.
- Electrocardiography . Pericarditis and effusion in the pericardium can produce distinctive signs on an electrocardiogram.

- A chest x-ray is often performed if pericarditis is suspected in order to determine the level of effusion in the pericardial bag. The shadow of the heart may appear to be enlarged if there is a large accumulation of fluid in the pericardial sac (pericardial effusion). However, most people with sudden (acute) pericarditis have normal chest X-rays, as often there is only a small exudate or no exudate.
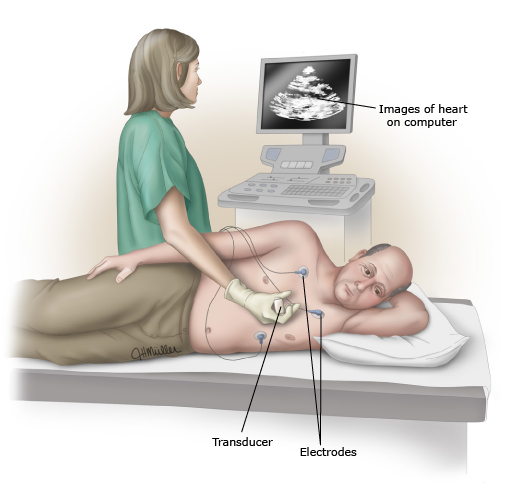
Additionally, ultrasound of the heart (echocardiography) is usually recommended, since it is a more sensitive test for detecting pericardial effusion. If there is a pericardial effusion, an echocardiogram can also help determine if the fluid limits the movement of the heart (i.e., causes tamponade of the heart). However, the absence of a pericardial effusion on an echocardiogram does not exclude the possibility of pericarditis.
When talking about pericarditis? At least two of the following four criteria are usually present in a person with pericarditis:
- Chest pain.
- Pericardial friction (abnormal heart sounds).
- ECG changes.
- Pericardial effusion on echocardiography or radiography.
Most people with pericarditis also have elevated blood levels of a substance called C-reactive protein (CRP) . This protein becomes elevated as a result of the inflammatory nature of pericarditis. CRP is particularly important for confirming suspicion of pericarditis and for monitoring the process of inflammatory disease and its response to therapy.
Video: 10 Signs of Pericarditis (Inflammation Around Heart)
Treatment of pericarditis in adults
There are practically no fundamental differences between the treatment of pericarditis in adults and in children. In both cases, the goals of pericarditis therapy include the relief of pain and the elimination of inflammation and effusion. You may also need special treatment for the cause of pericarditis.
Sometimes patients are examined in a clinic or hospital, and then treated at home, while others must remain in the hospital for the entire period of treatment. As a rule, upon admission to the hospital, it is recommended to carry out diagnostic tests in order to exclude a specific reason for which targeted therapy may be required, and not just an empirical anti-inflammatory effect. The risk of early complications should also be identified and eliminated (eg, fever, cardiac tamponade, large pericardial effusion, or recent treatment with anticoagulants such as warfarin (coumadin)).
Drug treatment of pericarditis in adults
Pain treatment . In most patients with acute pericarditis, treatment begins with taking aspirin or a non-steroidal anti-inflammatory drug (NSAIDs). It helps ease the pain. If the condition does not improve within one week, re-examination of the patient with a change in treatment regimen is necessary. Rest is also considered an important part of therapy, especially in the acute phase of the disease.
Another drug, colchicine , is recommended in addition to NSAIDs for most patients. In several studies, colchicine has been found to improve symptoms and reduce the risk of re-development of pericarditis.
If these drugs are useless or are not tolerated, hormonal drugs, such as prednisone, may be recommended. In most cases, the dose of steroids is maintained for several days, and then very slowly, over a period of weeks, the risk of recurrent pericarditis is reduced.
Treatment causes . When identifying the cause of pericarditis, treatment is directed to the underlying disease. For example, pericarditis caused by a bacterial infection will be treated with one or more antibiotics. However, viral pericarditis does not require any special antiviral treatment in most patients and is treated with empirical anti-inflammatory drugs. This is the reason why in all cases it may not be necessary to detect the causative virus.
Treatment of pericarditis in adults with myocardial infarction . Sometimes pericarditis and effusion in the pericardium occur as a complication of a heart attack (heart attack). Fortunately, the incidence of modern pericarditis with heart attacks has decreased dramatically due to modern treatment methods that minimize the extent of heart damage.
Pericarditis associated with a heart attack is usually temporary and lasts only a few days.
Another type of pericarditis, known as postcardiac injury syndrome, may develop several weeks or months after a heart attack, heart surgery, or other heart procedures. The best treatment for this condition is not fully understood. In different regions of the world, aspirin or a nonsteroidal anti-inflammatory drug is preferred (for example, ibuprofen or naproxen or naprosyn). Colchicine may be useful as an adjunct to another anti-inflammatory drug.
Pericardiocentesis
Pericardiocentesis is the medical term for determining the process of pericardial fluid removal using a thin needle.Pericardiocentesis can be recommended for patients who have pericardial effusion or cardiac tamponade (life-threatening complication of pericardial effusion). The procedure can be useful both as a treatment and as a method for determining the cause of pericarditis.

Risks of pericardiocentesis:
- Bleeding.
- Infectious lesion.
- Damage to the heart.
The risk of these complications can be minimized if pericardiocentesis is performed by an experienced doctor who performs the procedure on a regular basis.
Pericardiocentesis is usually done by inserting a needle through the skin into the pericardial sac and pericardial effusion.The needle is sent using ultrasound or X-ray (fluoroscopy). An ultrasound or fluoroscope allows the physician to determine where the pericardial effusion is located. The result is the exact direction of the needle. Less commonly, pericardocentesis is performed by incision and opening of the chest.
A small tube (drainage) often remains in place after the pericardiocentesis to allow fluid to flow out. If a certain amount of liquid remains in the pericardial bag, then a new liquid can continue to leak into the pericardial space. The catheter can remain inside the pericardium for one to two days or more, until almost or completely stop flowing out of the drainage fluid.
Pericardiectomy
Pericardiectomy is a surgical procedure during which part or most of the pericardium is removed. This method of treatment is radical, therefore it is used in the last turn and most often to eliminate recurrent pericarditis.
Pericardiectomy is associated with a small potential advantage and a greater risk of persistent pain. Postoperative complications may also occur. However, this type of treatment can be recommended in some situations after all other methods of exposure have been tried and have not done the desired result.
Complications of pericarditis
Approximately 15–30% of patients with sudden (acute) pericarditis have recurrent or persistent disease, often with a pericardial effusion. This risk is reduced in those who initially take colchicine and those who do not have a known cause of pericarditis (with idiopathic pericarditis).
The signs and symptoms of recurrent pericarditis are the same as in the initial progression of the disease.
Treatment of recurrent pericarditis is carried out by a medical method. This is usually used aspirin or nonsteroidal anti-inflammatory drug (NSAIDs), with the addition of colchicine to aspirin or NSAIDs. In addition, if there is a root cause, further evaluation and treatment is advisable.
Treatment with a hormonal drug (eg, prednisone) may be recommended if there is no response to these initial methods of exposure. However, the risk of recurrent pericarditis may increase with the use of steroids.
Side effects of steroids may include:
- Weight gain
- Development or worsening of diabetes.
- Increased risk of infection.
Thus, when steroids are used, the goal is to use the lowest possible dose as soon as possible. Nevertheless, the dose of the drug should remain constant until the symptoms disappear, and then it gradually decreases, which reduces the risk of further relapses.
Dealing with recurrent pericarditis can be quite debilitating and time consuming. Therefore, it is important for the patient to discuss with the doctor the nature of the disease, its presumptive development and alternative treatment options. In particular, the following features of pericarditis, which recurs, can be noted:
- After successful treatment of recurrence, the disease may develop again. This process can be repeated at different intervals over a long period, up to several years. However, relapses are most common during the first one to two years and tend to become less and less and less severe in most cases.
- The cause of pericarditis, if known, should be treated first. If the first disease was caused by a virus, reinfection with this virus is unlikely to occur, so there will be no recurrence. The disease eventually disappears just as mysteriously as it appeared, and almost always occurs without permanent complications.
Heart tamponade and constrictive pericarditis are serious but rare complications of recurrent pericarditis. Symptoms of cardiac tamponade include shortness of breath, weakness, and chest pain. Symptoms of constrictive pericarditis include swelling of the legs and other parts of the body, fatigue and shortness of breath. Such complications are extremely rare for idiopathic cases, when specific causes are excluded (for example, bacterial and neoplastic pericarditis).
It is important to remember about the likelihood of developing cardiac tamponade and other complications of pericarditis, and take all necessary precautions to prevent their development.
Video: Treating Pericarditis-Mayo Clinic
