Heart pacemaker: indications for surgery
Author Ольга Кияница
2018-07-24
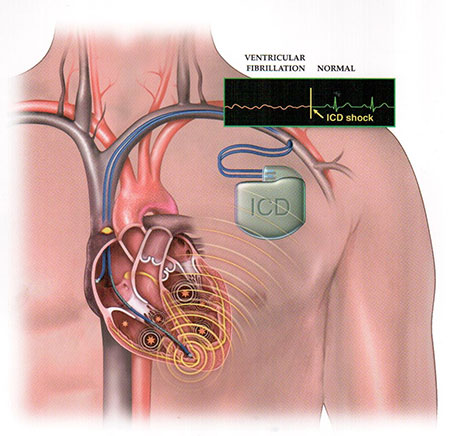
Pacemakers (CS) are medical devices that stimulate the heart with the help of electrical impulses. Used to maintain or restore a normal heart rhythm.
In 1958, the first permanent pacemaker was implanted, after which the popularity of the installation of such a device began to increase steadily. It is estimated that more than 300,000 patients in the United States annually receive a permanent pacemaker, and about 900,000 pacemakers are implanted worldwide.
Indications for the use of a pacemaker have significantly expanded over the past 45 years and today include the treatment of bradyarrhythmias and electrotherapy of tachyarrhythmias, certain types of fainting and progressive heart failure. Device technology also evolved from simple single-chamber pacemakers with fixed speed to multi-chamber, responsive to speed (to meet physiological needs), capable of stimulation, cardioversion and defibrillation.
Video: What diseases do you need a pacemaker?
Description of pacemakers
Since the creation of the first pacemaker, several significant improvements have been made. In addition, a modern permanent pacemaker is a subcutaneously placed device. There are 3 types of artificial pacemakers:
- Implantable pulse generators with endocardial or myocardial electrodes.
- External, miniature, portable stationary, battery-powered, which are pulse generators with external electrodes for temporary transfusion endocardial or transthoracic myocardial stimulation.
- Cardioverters or monitors with AC power supply with high-current external transcutaneous or low-current endocardial or myocardial regimens for temporary stimulation in asynchronous regimens or modes with manual or initiated stimulation.

All pacemakers consist of two components: a pulse generator that provides an electrical impulse to stimulate the myocardium, and one or more electrodes / wires that impart an electrical impulse from the generator to the myocardium.
The decision to introduce a pacemaker is usually based on the symptoms of bradyarrhythmia or tachyarrhythmia. Symptomatic bradycardia is the most common indication.
Other symptoms that result from severe bradycardia include fatigue, reduced physical activity and overt heart failure. Physiological sinus bradycardia, which is often determined by highly skilled athletes, is not an indication for the installation of an electrical heart stimulant.
Indications for pacemaker implantation
The most common indications for a permanent CS are dysfunction of the sinus node and a complete atrioventricular (AB) blockade. Operations to install the COP are conducted according to guidelines developed by the target group: American College of Cardiology (ACC), American Heart Association (AHA) and Heart Rhythm Society (HRS). The Society of Cardiologists, operating in Europe, has developed similar recommendations.
ACC / AHA / HRS divides the indications for the implantation of a pacemaker into 3 classes:
- Class I: Pacemaker implantation is considered necessary and useful (the benefits are much greater than the existing risks).
- Class II: divided into two subclasses:
- IIa - the value of evidence in favor of effectiveness (benefit greater than risk) is greater;
- IIb - the effectiveness of implantation of CS is less substantiated (the benefit exceeds or equal to the risks).
- Class III: permanent stimulation is not recommended, and in some cases it may be harmful (risks exceed benefits).
The following conditions are included in the ACC / AHA / HRS recommendations for the pacemaker installation. Class I and II recommendations should be discussed first.
- Dysfunction of the sinus node.
- Acquired atrioventricular block.
- Chronic bifascicular blockade.
- After acute myocardial infarction.
- Neurocardiogenic syncope and hypersensitive carotid sinus syndrome.
- Postcardary transplantation.
- Hypertrophic cardiomyopathy.
- Pacing for the detection and cessation of tachycardia.
- Cardiac resynchronization therapy in patients with severe systolic heart failure.
- Patients with congenital heart disease.
Sinus node dysfunction
Indications I class
- Fixed symptomatic sinus bradycardia, as well as frequent pauses in the work of the sinus node, which cause symptoms of the disease on the background of drug therapy to improve the clinical condition.
- Symptomatic chronotropic incompetence (inability to achieve 85% of the predicted maximum age of heart rate for a formal or informal positive stress test or the inability to determine the age-related heart rate during a normal lifestyle).
Indication class II
- Sinus bradycardia with heart rate less than 40 beats per minute, but without a clear connection between the symptoms and the disease itself.
- An unexplained syncope, when clinically significant disorders of sinus node activity are detected or provoked by electrophysiological (EP) studies.
- Minimally symptomatic patients with chronic heart rate less than 40 beats / min during wakefulness.
Acquired atrioventricular block
Indications I class
- Complete blockade of the AV-node of the third degree with a pronounced clinic or without it.
- Symptomatic blockade of the second-degree AV node, type Mobits I and II.
- AV blockade of the second or third degree, caused by physical exertion, in the absence of myocardial infarction.
- Mobitz II with enlarged ventricular complexes.
Indication class II
- Asymptomatic type Mobitz II with a narrow complex of QRS.
- Blockade of the AV node of the first degree, when there is a hemodynamic compromise.
- Asymptomatic AV-blockade of the second degree.
Chronic bifascicular block
Indications I class
- Extended AV blockade of the second degree or intermittent AV blockade of the third degree.
- Variable blockade of the branch.
- Blockade of the AV node of the second degree.
Indication class II
- Fainting with suspicion of blockade of the AV node with the exclusion of other probable causes, in particular ventricular tachycardia.
- Accidental detection during diagnosis of a highly elongated HV interval (> 100 ms) or triggered by stimulation of a blockade within the bundle of the His in asymptomatic patients.The HV interval is the conductivity time from its bifurcation, located just below the AB node, to the first identifiable start of ventricular activation.
- Can be considered in patients with neuromuscular disease such as myotonic muscular dystrophy, Erb's dystrophy and fibular muscular dystrophy with bifascicular blockade or any fascial blockade with or without a clinic.
After acute myocardial infarction
Indications I class
- Constant stimulation of the ventricles with stable blockade of the AV node of the second degree in the Gisa-Purkinje system with alternating blockade of branches or AB blockade of the third degree inside or below the Gisa- Purkinje system after ST-segment elevation.
- Constant stimulation of the ventricles with a progressive progressive block of the second or third level of the inferior AV blockade and associated blockade of the branches.
- Constant stimulation of the ventricles with stable and symptomatic AV-blockade of the second or third degree.
Indication class II
- Constant stimulation of the ventricles can be considered as an indication for an asymptomatic constant AV block of the second or third degree at the level of the AV node.
Neurocardiogenic syncope and hypersensitive carotid sinus syndrome
Indications I class
- Recurrent syncope caused by spontaneous carotid artery stimulation and carotid artery pressure, which causes ventricular asystole more than 3 seconds.
Indication class II
- Fainting without an obvious and provocative event, and with a hypersensitive cardioinhibitory response lasting 3 seconds or more.
- Significant symptomatic neurocardiogenic syncope associated with bradycardia, recorded spontaneously or when performing a test with an inclined table.
Postcardiac transplantation
Indications I class
- Persistent inadequate or symptomatic bradycardia without self-permission, and other indications of the first class with constant stimulation.
Indication class II
- Definition of relative bradycardia, which is prolonged or recurrent, which limits the rehabilitation or positive changes in the period of postoperative recovery.
- The presence of syncope after cardiac transplantation, even when the bradycardia was not fixed.
Hypertrophic cardiomyopathy
Indications I class
- Patients with hypertrophic cardiomyopathy who have dysfunction of the sinus node or AV blockade.
Indication class II
- In the presence of severe refractory symptoms with hypertrophic cardiomyopathy and with a significant stop or provocation of obstruction of the outflow of the left ventricle.
Pacemaking for the detection and cessation of tachycardia
Indications I class
- The presence of a sustained pause, depending on the ventricular tachycardia, with or without QT prolongation.
Indication class II
- It is recommended for patients with a high risk of developing congenital syndrome of the extended QT segment.
- It can be considered for the purpose of preventing symptomatic, drug refractory recurrent atrial fibrillation in patients with concomitant disruption of the sinus node.
Cardiac resynchronization therapy in patients with severe systolic heart failure
Indications I class
- If there is a left ventricular ejection fraction (LVEF) of less than or equal to 35%, sinus rhythm, blockade of left branch of the left bundle, type I symptoms, optimal medical therapy with a QRS score greater than or equal to 150 ms, cardiac resynchronization therapy (CPT) with or without implantation of CS.
Indication class II
- LVEF is less than or equal to 35%, sinus rhythm, BVLP with symptoms of class III or IV, and with optimal medication and QRS duration from 120 to 149 ms, CPT is recommended with or without CS implantation.
- LVEF is less than or equal to 35%, sinus rhythm, non-BVLP sample with QRS greater than or equal to 150 ms, and symptoms of class III / outpatient class IV with a focus on medication.
- Patients with atrial fibrillation and LVEF are less than or equal to 35% in medical therapy if the patient needs ventricular stimulation or otherwise meets the criteria for CPT, with the ablation of the AV blockade or the pharmacologic regulation of the heart rate that can control about 100% of ventricular stimulation with CPT.
- LVEF is less than or equal to 35%, grade III or IV symptom with optimal medical therapy and frequent dependence on ventricular stimulation, while CPT is reasonable.
Congenital heart disease
Indications I class
- Progressive blockade of the AV node of the second or third degree with concomitant symptomatic bradycardia, impaired ventricular function or low cardiac output. Also a progressive AV block of the second or third degree, which is expected to not be resolved or persists for 7 days or longer after cardiac surgery.
- Dysfunction of the sinus node with correlation of signs during pronounced bradycardia.
- Congenital blockade of AV-node of the third degree with a wide ventricular complex, complicated ventricular ectopia or ventricular dysfunction.
- Congenital blockade of the AV node of the third degree with a frequency of ventricular contractions is less than or equal to 55 beats / min or with congenital heart disease with a ventricular contraction rate less than or equal to 70 beats / min.
Indication class II
- Congenital heart defects combined with sinus bradycardia in order to prevent recurrent episodes of atrial atrial tachycardia, while dysfunction of the sinus node may be integral or secondary to antiarrhythmic treatment.
- Congenital blockade of the AV node of the third degree in the first year of life with an average heart rate of less than 50 beats per minute, with sharp pauses during contractions of the ventricles, which are 2 or 3 times the main cycle length or are associated with symptoms due to chronotropic incompetence.
- The transient postoperative blockade is AV-Uzala of the third degree, which is restored to a sinus rhythm with residual bifascicular blockade.
- Asymptomatic sinus bradycardia after biventricular restoration of congenital heart disease in patients with a heart rate of less than 40 beats / min or with pauses in ventricular velocity more than 3 seconds.

Contraindications
As in any procedure, the pacemaker implantation should be carried out selectively depending on the condition of the individual patient. There are situations when the CS installation is not as useful as expected, or insufficient indications for its use. Sometimes they are also called class III indications in the ACC / AHA / HRS guidelines or the guidelines of the European Society of Cardiology.
- Sinus bradycardia without significant symptoms; asymptomatic AV-blockade of the first degree.
- AV blockade, which is not expected to be allowed or can repeat the example of drug toxicity, Lyme disease or temporary increase in vagal tone.
- A pacemaker is not indicated for sinus node dysfunction in patients with symptoms indicating bradycardia that have been reported even in the absence of a bradycardia.
- Asymptomatic Mobic of the second degree, blockade of type I.
- Asymptomatic long RR interval with atrial fibrillation or other causes of transient ventricular pauses.
- Hypersensitive cardioinhibitory response to stimulation of the carotid sinus in the absence of symptoms or in the presence of vague symptoms, such as dizziness.
- Asymptomatic bradycardia during sleep.
- CPT is not indicated in patients whose functional status and longevity are limited primarily to non-cardiac conditions.
- Blockade of branches of the right bundle with a deviation of the axis to the left without fainting or other symptoms compatible with intermittent AV blockade.
- Syndrome of elongated QT or pirouette tachycardia due to reversible causes.
- The presence of an auxiliary pathway, which is capable of rapid anterograde conduction.
- Definition of symptoms of class I or class II and non-VLP with a QRS duration of less than 150 ms.
Video: Pacemakers
Similar articles

The most critical conditions are considered shock, because with their development a person can die very quickly. If emergency care is not provided, including cardiogenic shock, death occurs within a few minutes. The occurrence of a violation is primarily associated with cardiovascular diseases.

The process of pacemaker installation is not as complicated as it may seem. Today, this manipulation is equated to an operation to remove appendicitis. More questions arise in patients how to live, after the installation of ACS, but the process of surgical intervention itself is important.

Some forms of rhythm disturbance may pose a risk of sudden cardiac arrest. In such cases, doctors recommend a pacemaker that regulates cardiac activity. In order to better imagine a way of life with an artificial driver of rhythm, you need to know the principle of operation of the device.
