Eclampsia of pregnant women: symptoms, diagnosis and treatment
Author Ольга Кияница
2018-09-26
Eclampsia (or late toxicosis of pregnant women, PTB) is the highest stage of development of preeclampsia associated with a sharp and significant increase in blood pressure, while protein is often detected in urine. In such cases, talking about hypertension and proteinuria. With eclampsia, convulsions occur that can bring a woman and fetus to death.
The term “eclampsia” comes from the ancient Greek. λκλαμψις, which means flash, a sudden appearance.
According to wikipedia.org.
Pre-eclampsia and eclampsia in pregnant women are determined, in some cases, it progresses up to delivery and the postpartum period. In case of severe preeclampsia, an emergency obstetric aid is performed, since most often after removal of the child from the womb of the mother, the attacks of eclampsia stop.
Video: Preeclampsia & eclampsia - causes, symptoms, diagnosis, treatment, pathology
Description of eclampsia and preeclampsia
Eclampsia is the development of seizures in a woman against the background of severe pre-eclampsia. This condition has 2% mortality. Preeclampsia and eclampsia are most common in the first pregnancy. Pregnant adolescents and women over 40 are more likely to develop these pathologies.
Preeclampsia (PE) is a condition that can develop during pregnancy, characterized by high blood pressure (hypertension) and protein in the urine (proteinuria). If the condition is not properly recognized and appropriate treatment is not given, preeclampsia can progress to eclampsia. Eclampsia is serious for both mother and child, and can even be fatal. Pre-eclampsia was previously known as pregnant women’s toxemia. According to statistics, one woman out of 200 cases of preeclampsia without seizures, convulsions (eclampsia) occur without treatment. Estimates of the prevalence of preeclampsia range from 2 to 7% among clinically healthy women who have not given birth before.
Preeclampsia mainly occurs after the 20th week of pregnancy and can be observed within 48 hours after the birth of a child. Sometimes pre-eclampsia is determined 4-6 weeks after birth. In most cases, occurs after the 34th week of pregnancy, and in 6% - after birth.
Pathogenesis of preeclampsia
It is associated with impaired implantation of the egg in the uterus wall (myometrium). From the figure below, it can be seen that, against the background of ischemia , inflammatory mediators, as well as angiotensin and placental factors, are being actively produced. As a result, the endothelium is damaged, the compensatory mechanisms gradually disappear and the placenta begins to “artificially” increase the missing pressure to improve the blood supply to the fetus.Against this background, changes in blood pressure of the pregnant woman with all the ensuing consequences. The resulting conflict leads to endothelial dysfunction.
 In severe cases, the endothelium begins to be affected throughout the body. Developed systemic endothelial dysfunction, causing disruption of many vital organs. Thus, conditions are created for the occurrence of pre-eclampsia, and after - eclampsia.
In severe cases, the endothelium begins to be affected throughout the body. Developed systemic endothelial dysfunction, causing disruption of many vital organs. Thus, conditions are created for the occurrence of pre-eclampsia, and after - eclampsia.
Blood pressure value
The pressure inside the arteries is created so that blood can circulate throughout the body to deliver oxygen and other nutrients. This process ensures the normal metabolism and functioning of the whole organism.
The blood pressure indicator identifies the pressure inside the arteries as two values - upper and lower. The first, or upper, value is defined as systolic pressure and indicates the pressure arising from the contraction of the heart to pump blood through the arteries. The second, or lower, value is diastolic pressure, indicating the pressure inside the arteries, when the heart relaxes and fills with blood.
Inside the arterial blood vessels there must be a major pressure, regardless of whether the heart is contracting or not.This internal pressure is maintained by the smooth muscle muscles, which forms the walls of the arteries, large and small, and, in fact, is compressed and maintains vascular tone.
The normal blood pressure in a normal state is less than 120/80, while 120 is systolic blood pressure and 80 is diastolic blood pressure.
Causes and risks
The exact cause of preeclampsia and eclampsia is not fully understood, but it is believed that this disorder is associated with impaired vascular tone. Anomalies of the placenta are also described. Most of all, there is a combination of etiological factors, including both genetic and environmental impact measures. Several genes have been studied that promote the development of preeclampsia. They significantly increase the risk for women who have other family members with eclampsia or preeclampsia.
Eating disorders, obesity, and disorders of the immune system may also play a role in the development of pathological conditions, although this is not fully understood. Some studies of immune responses during the development of preeclampsia have shown that certain cells of the immune system interact with each other to regulate the immune response.
Major risk factors for preeclampsia and eclampsia
Various factors may increase the risk of a woman having pre-eclampsia and eclampsia. These include:
- Age (in adolescence or in women over 40 is more likely to suffer from PE and eclampsia).
- Positive case history associated with preeclampsia or eclampsia during the development of a previous pregnancy.
- Overweight.
- The presence of high blood pressure before pregnancy.
- Pregnancy has occurred as a result of using a donor egg or fertilization with donor sperm.
- In the family, women already had preeclampsia.
- A history of the disease identifies diseases such as diabetes, systemic lupus erythematosus, rheumatoid arthritis or kidney disease.
- Multiple pregnancy.
- Sickle cell anemia.
Symptoms
Most women with mild preeclampsia have no clinical manifestations of the disease. Key features, as mentioned earlier, are:
- The presence of protein in the urine (proteinuria).
- Increased blood pressure (hypertension).
- Women with preeclampsia may experience a sudden weight gain for 1-2 days.
- Swelling of the legs and arms, which can be spread to other parts of the body, with these symptoms may occur during normal pregnancy and are not necessarily associated with preeclampsia.
Other symptoms and signs that may occur with severe pre-eclampsia:
- Dizziness.
- Headache.
- Nausea.
- Vomiting.
- Abdominal pain.
- Vision changes.
- Upset reflexes
- Mental state disorder.
- Fluid in the lungs (pulmonary edema).
- Decreased urine output (partial - oliguria, full - anuria).
Symptoms of eclampsia include manifestations of preeclampsia along with the development of seizures, first tonic and then clonic. When seizures occur, they are most often preceded by neurological disorders such as headaches and visual disturbances. In women with severe pre-eclampsia, a reduced platelet count (below 100,000) can be detected.
The signs and symptoms of pre-eclampsia self-reduce and disappear within 1-6 weeks after delivery.
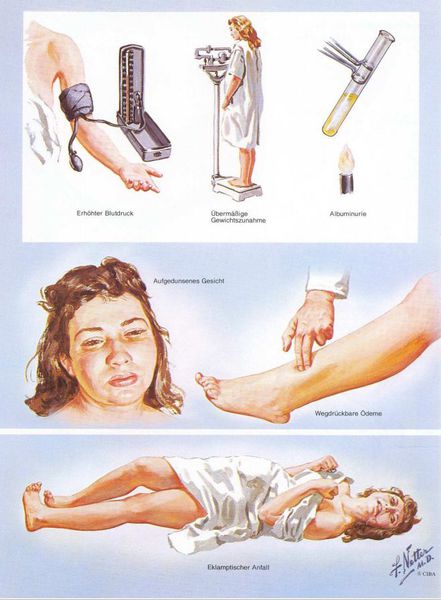
A visual depiction of the manifestations of preeclampsia was presented by Frank Henry Netter, a surgeon and illustrator.
Diagnostics
Preeclampsia can be diagnosed by regularly screening a pregnant condition.
- A urine protein is diagnosed using a general urine test.
- Measurement of blood pressure at each visit to the clinic makes it possible to monitor this indicator. Blood pressure in preeclampsia usually exceeds 140/90.
- Blood tests with blood cell counts and blood clotting tests can be performed. Recent studies have shown that congo red (CR) spotting tests may be better indicators of preeclampsia than standard urine tests for proteinuria. The test is based on the fact that the urine and placenta of women with preeclampsia contain abnormal proteins that bind to the red substance of the Congo.
Since preeclampsia can be asymptomatic (cause no changes), it is important for pregnant women to undergo regular medical examinations. Also conducted instrumental research methods to monitor the health of the mother and child (echocardiography, phonocardiography, etc.).
There are no prognostic tests for today, so it is not yet possible to predict with maximum certainty whether a woman will develop preeclampsia or not.
Video: 4 Stages of Eclampsia
Treatment
The most effective treatment of preeclampsia and eclampsia is one - emergency delivery. The question of whether it is necessary to stimulate uterine contraction or perform a cesarean section depends on the severity of the condition, as well as on the gestational age and well-being of the fetus.
In women with mild preeclampsia, labor is most often stimulated at week 37. Until that time, they may be at home or in the hospital with careful monitoring. To control the condition, steroid drugs are used to improve the maturation of the child’s lungs. Women with mild pre-eclampsia before the onset of 37 weeks most often must adhere to bed rest with constant medical supervision.
In severe preeclampsia, obstetrics (induction of labor or cesarean section) is usually seen after 34 weeks of gestation.The risks to the mother and child of the disease must be balanced with the risk of prematurity in each case separately.To prevent seizures, women with severe pre-eclampsia are given intravenous magnesium sulfate. This medicine is safe for the fetus. Magnesium supplementation tablets are not effective in preventing seizures, so they are generally not recommended. Additionally, medications, such as hydralazine, may be used to help lower blood pressure.
Eclampsia requires emergency medical care. Pathology is treated with drugs to control seizures and maintain a stable blood pressure in order to minimize complications for both the mother and the child. Magnesium sulphate is used primarily, especially when eclamptic seizures develop. If magnesium sulfate is not effective, other drugs may be used, such as lorazepam (ativan) and phenytoin (dilantin).
Complications
Preeclampsia causes a decrease in blood flow to the placenta and fetus. Thus, a baby can cause growth retardation and weight loss at birth. Early delivery is also quite common and not all children normally perceived.
Oligohydramnios , a decrease in the volume of amniotic fluid, is a frequent accompaniment of preeclampsia. This condition also increases the risk of placental abruption or separation of the placenta from the walls of the uterus. With severe development, life-threatening bleeding and fetal death can occur.
Severe preeclampsia can affect liver and kidney function. HELLP syndrome, hemolysis (destruction of red blood cells), increased activity of liver enzymes (destruction of the parenchyma) and low platelet count is a rare complication of preeclampsia, but very serious. Symptoms include headache, nausea, vomiting, and pain in the right side or upper quadrant. In some cases, HELLP syndrome develops before the appearance of typical signs of preeclampsia. Other unusual complications of pre-eclampsia and eclampsia include a decrease in blood flow in the brain, which leads to a stroke.
Prevention and prognosis
Today it is not fully known how to prevent preeclampsia and eclampsia. However, the results can be improved by the prompt recognition and application of appropriate therapies. In this regard, pregnant women should undergo regular health screenings in a timely manner.
Predictive conclusion
Most women with mild preeclampsia have a good prognosis regarding the termination of pregnancy. Eclampsia is a serious disease with a high mortality rate of around 2%.
The risk of recurrence in preeclampsia varies depending on the onset and severity of the condition. Women with severe pre-eclampsia who are advised to have early childbirth are most at risk of relapse. For such cases, studies show that the recurrence rate is between 25% and 65% for this population.
It was determined that 5-7% of women with mild preeclampsia will have preeclampsia during subsequent pregnancy.
Women with preeclampsia may be at increased risk of cardiovascular disease for later life. This risk is greatest in women with early onset severe pre-eclampsia.
Video: Eclampsia
Similar articles

Pulse is an important biomarker of the body's condition, which is why every woman in the situation is important to know the rate of the pulse, as well as those changes that appear, you should immediately consult a doctor. Especially the information is relevant for those who believe that they are all right with the heart and blood vessels.
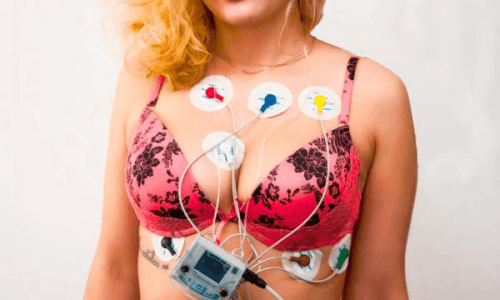
During pregnancy, there are various physiological changes, especially those relating to the cardiovascular system of women. With the help of electrocardiography, some of them can be seen already in the first trimester. To understand whether the pregnancy is normal or there are abnormalities, the decoding of the ECG is carried out.

Arterial pressure, which increases in a pregnant woman, requires detailed and continuous monitoring. Pathology can proceed favorably, but sometimes severe conditions occur that threaten the life of the mother and child.
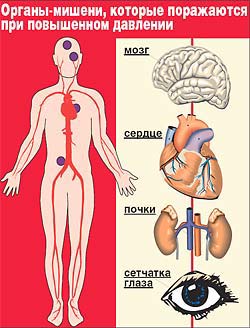
Many people around the world are suffering from an illness such as arterial hypertension. Other common names of the disease are hypertension, hypertension, hypertension. Unfortunately, such a pathology is very often determined in pregnant women. With timely treatment it is possible to improve the condition of patients and to prevent serious complications.
