Transient ischemic attack
Author Ольга Кияница
2018-05-11
Transient ischemic attack (TIA) is an acute episode of temporary neurological dysfunction, which occurs as a result of focal involvement of the cerebral, spinal cord or ischaemia of the retina and is not associated with acute myocardial infarction. Clinical TIA symptoms are usually observed for less than 1 hour and most often last for no more than 30 minutes. In rare cases, long episodes of an attack can occur.
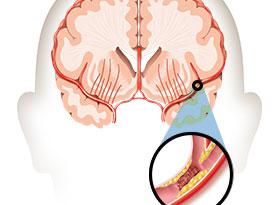
Transient ischemic attack most often develops against the background of atherosclerotic occlusion of large cerebral vessels, that is, when atherosclerotic plaques completely overlap the bloodstream at the site of the branching of the carotid arteries, the internal carotid artery or vertebral arteries.
The basis for the assessment of TIA lies in the neurological examination of the patient, which focuses on neurovascular diagnosis. Also, the presence of other diseases that can complicate the TIA's course is taken into account. As soon as intracranial hemorrhage is excluded, antithrombotic therapy begins.
TRANSITIC ISHEMIC ATTACK - PREVENTION OF THE INSULATION
Description
At first, the classic definition of transient ischemic attack included symptoms up to 24 hours. Subsequently, using such diagnostic techniques as neuroimaging, it was suggested that many of these cases are minor changes with characteristic symptoms, and not with true TIA. Thus, in 2009, the American Heart Association (AHA) and the American Stroke Association (ASA) approved the diagnosis of TIA based on a histological study (i.e., as an episode of focal ischemia and not an acute myocardial infarction). [1 - Easton JD; Saver JL; Albers GW; Albert MJ; Chaturvedi S;Feldmann E; Hatsukami TS; Higashida RT; Johnston SC; Kidwell CS; Lutsep HL; Miller E; Sacco RL. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association / American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council is Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke 2009; 40 (6): 2276-93]
TIA is characterized by a temporary decrease or cessation of cerebral blood flow through the vessels as a result of partial or complete occlusion. As a rule, this is due to acute thromboembolic disease or stenosis of the vessel.
Statistics on transient ischemic attack:
- In the US, between 200,000 and 500,000 primary TIAs are diagnosed annually. [2 - Kleindorfer D; Panagos P;Pancioli A; Khoury J; Kissela B; Woo D; Schneider A; Alwell K; Jauch E; Miller R; Moomaw C; Shukla R; Broderick JP.Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 2005; 36 (4): 720-3]
- During TAI treatment, the patient is diagnosed in 0.3% of cases.
- TIA, by its development, greatly enhances the short-term risk of stroke, as approximately 15% of diagnosed strokes are preceded by TIA.
- In developed countries, the probability of occurrence of primary TIA is about 0.42 per 1000 population. TIA is determined by approximately 150,000 patients a year in the UK.
- The incidence of TIA increases with an age range of 1-3 cases per 100,000 people under the age of 35 years to 1,500 cases per 100,000 people over the age of 85 years.
- Less than 3% are for children. Pediatric cases often have a completely different etiology in comparison with TIA in adults.
- The incidence of TIA in males (101 cases per 100,000 population) is significantly higher than in females (70 per 100,000).
Reasons
There are many potential causes of transient ischemic attack, among which the following are of particular importance for adults:
- Atherosclerosis of extracranial drowsiness and vertebral or intracranial arteries
- Sources of embolic defects, which include valve disease, ventricular thrombus, or thrombus formation during atrial fibrillation, arterial aortic disease, paradoxical embolism through a patented oval hole or defect of the atrial partition
- Arterial dissection
- Arteritis - inflammation of the arteries, mainly in the elderly, especially women; non-infectious necrotizing vasculitis (primary cause); taking some medicines; irradiation; local trauma; connective tissue diseases
- Sympathomimetic drugs (for example, cocaine)
- Massive lesions (for example, tumors or subdural hematomas) - they are not so often caused short-term symptoms and often lead to a progressive stable clinic
- Hypercoagulation states (for example, genetic, associated with cancerous infection or infection)
Causes of TIA development in children:
- Congenital heart defects with cerebral thromboembolism (most often)
- Drug addiction (for example, cocaine)
- Disruption of blood coagulation
- Infection of the central nervous system
- Neurofibromatosis
- Vasculitis
- Idiopathic progressive arteriopathy
- Fibromuscular dysplasia
- Marfan's disease
- Tuberculous sclerosis
- Tumor
- Sickle cell anemia
- Focal Arteriopathies
Clinic
Symptoms of TIA often develop suddenly. They are identical to those that are inherent in ischemic stroke, but are temporary and reversible. Their duration usually ranges from 2 to 30 minutes, after which they are completely resolved.
A patient may have several TIA for 1 day or only two or three times in a few years.
The TIA Clinic may include the following sudden signs:
- Weakness or paralysis on one side of the body (for example, half the face, one arm or leg or all one side)
- Loss of sensation or abnormal sensation on one side of the body
- Difficulty of speech (for example, vague speech)
- Confusion, hardly understandable speech
- Darkening, blurring or loss of vision, especially in one eye
- Dizziness or loss of balance and coordination

Clinical evaluation of a possible TIA involves careful study of the onset of the disease, duration, fluctuation, location, and severity of symptoms. A review of the patient's medical record is imperative, which is extremely important in detecting dysfunction from previous attacks, seizures or heart attacks.
Clinical manifestations will vary depending on the vessel involved and the magnitude of the area of the brain that it enriches with blood.
Initially, an exception is made to emergency situations that may imitate TIA:
- Hypoglycemia
- Tumor or massive lesion
- Migraine with aura
- Disturbance of the peripheral nerve
- Demyelinating disease
- Vestibular dysfunction
- Intracranial hemorrhage
- Electrolyte disorders
TIA may last for several minutes, with symptoms often disappearing before the patient examined the doctor. Thus, questions related to the history of the disease are often asked not only to the patient, but also to his family members, witnesses or emergency medical staff.
Video Transient cerebral circulation disorder
Diagnostics
Initially, the following vital indicators are studied:
- Temperature
- Blood pressure
- Heart rate and rhythm
- Respiratory rate
- Oxygen saturation
In the process of assessing the general condition and appearance of the patient, it is studied:
- Carefulness
- Ability to interact with others
- Language skills and memory skills
- Total hydration level
- General development
The purpose of the physical examination is to identify any neurological changes, to evaluate the risk factors for cardiovascular diseases, and to search for a potential thrombotic or embolic attack source. Ideally, any neurological disorder should be recorded using locomotor tests (TWT, Hauser) and integral scales (ADL, F1M).
During a neurological examination, the following is investigated:
- Function of cranial nerves
- Determination of the somatic strength of the engine
- Somatic sensory testing
- Testing speech and language
- Evaluation of the cerebellar system (be sure to observe the patient's progress)
It is important to exclude other causes, such as metabolic or drug-induced factors, which may be manifested by symptoms similar to those of the TIA.
In addition, the following studies are prescribed:
- Blood glucose analysis
- General blood test
- Number of electrolytes in serum
- Coagulogram
- Standard electrocardiogram
The following analyzes can be carried out urgently:
- Reduction rate of red blood cells
- Heart Enzymes
- Lipid profile
If necessary, additional laboratory tests are carried out, which include:
- Screening of hypercoagulation states
- Serology of syphilis
- Antiphospholipid antibodies
- Toxicological factors
- Electrophoresis of hemoglobin
- Electrophoresis of serum
- Investigation of cerebrospinal fluid
Diagnostic tools allow you to get a brain image, only they must be performed within 24 hours of the onset of symptoms:
- Magnetic resonance imaging (MRI) with diffusion-weighted imaging (preferably)
- Computed tomography (CT, ordered, if MRI is not available)
Visualization of the cerebral vascular system is often done urgently, very desirable, in conjunction with the visualization of the brain. Vascular visualization for TIA includes the following:
- Color Doppler ultrasonography
- CT Angiography (CTA)
- Magnetic resonance angiography
Thus, timely and extensive diagnostics allows you to accurately diagnose and carry out highly effective therapy.
Treatment
Before appointing patients with TIA appropriate treatment, the following is done urgently:
- Assessment of the general condition of the patient
- Stratification of risk
- Initiation of stroke prevention
For patients with a recent (≤1 week) TIA, immediate hospitalization is recommended, especially with the following indications:
- The duration of the symptoms is longer than 1 hour
- There are signs of stenosis of the carotid artery more than 50%
- There is a reliable source of embolism (for example, atrial fibrillation)
- The hypercoagulation state is determined
Due to the high short-term risk of stroke after TIA, antithrombotic drugs are prescribed only after elimination of intracranial hemorrhage. Appropriate first line option for initial therapy:
- Aspirin
- Aspirin plus dipyridamole with prolonged release
- Clopidogrel
The treatment plan for stroke prevention is usually recommended with cardioembolic TIA and looks like this:
- For patients with atrial fibrillation after TIA, long-term anticoagulation with warfarin and aspirin is prescribed, if someone can not take oral anticoagulants
- In acute myocardial infarction and thrombus of the left ventricle, oral anticoagulation with warfarin in combination with aspirin is prescribed.
- With extended cardiomyopathy, oral anticoagulation with warfarin or antiplatelet therapy is performed.
- At rheumatic disease of a mitral valve an oral anticoagulation with warfarin is performed
Patients with TIA due to 50-99% of the stenosis of the main intracranial artery, the following is recommended:
- Aspirin, not warfarin
- Maintenance of arterial pressure below 140/90 mm Hg. Art. and the total cholesterol level is below 200 mg / dl
Surgery
If the patient is considered to be at increased risk (for example, if the carotid artery is narrowed by at least 70%), an artery expansion (a so-called carotid endarterectomy) can be performed to improve the patient's condition.
Carotid endarterectomy usually involves the removal of fatty deposits (atheroma or plaque) formed due to atherosclerosis and clots in the internal carotid artery. However, the operation can cause a stroke, because in the process of its implementation, clots or other material is often supplanted, which is then able to spread with the bloodstream and block the artery. However, after surgery, the risk of stroke decreases for several years than when using drugs.

Stents
If a patient is contraindicated in surgery, an angioplasty with stenting may be required. For this procedure, the catheter with a balloon on its tip is introduced into the narrow artery. Then the balloon is filled with air, it blows in a few seconds, which helps to expand the artery. In order to prevent the vessel from being stenosed after this, doctors insert a tube from a wire mesh (stent) into the artery.
Prevention
Despite the lack of reliable studies demonstrating the effectiveness of lifestyle changes with a view to preventing TIA, many health professionals recommend them. These include:
- No bad habits (smoking)
- Reducing fats to help reduce the number of plaque formation
- Keeping a healthy diet that includes lots of fruits and vegetables
- Restriction of sodium in the diet, which helps to lower blood pressure
- Dosage consumption of alcohol, stimulants, sympathomimetics, etc.
- Maintaining healthy weight
In addition, in the presence of cardiovascular disease, it is important to keep them under control, especially if these are the following pathological conditions:
- High blood pressure
- High cholesterol
- Atrial fibrillation
- Diabetes mellitus
Forecast
The early risk of a stroke after a transient ischemic attack is approximately 4% in 2 days, 8% in 30 days and 9% in 90 days. In prospective trials of patients on TIA, it was found that the incidence of stroke reaches 11% in 7 days. Probability of stroke within 5 years after TIA is 24-29%. In addition, patients with TIA or stroke have an increased risk of coronary artery disease.
Video Prevention of recurrent stroke and TIA
