Angina of tension
Author Ольга Кияница
2019-02-02
Angina pectoris is a clinical syndrome, which includes various symptoms, among which the most important - redness pain. In some cases, patients only notice discomfort in the chest. But at the same time the disease can be as dangerous as with severe pain.
For the first time, angina was described by English physician William Heberden.
Accordingly, WHO classification from 1979, angina pectoris can occur in a calm and tense manner. The second form of the disease is less favorable, as it is more often complicated by myocardial infarction.
Video: Unstable Angina ¦ Treatment and Symptoms
Description of angina pectoris
Unstable angina pectoris is a type of acute coronary syndrome that can hold one or more symptoms. At the same time, the level of heart biomarkers detected in the blood does not meet the criteria for determining acute myocardial infarction (MI).
According to various data, the greatest risk of angina is 65-74 years (up to 20%), whereas in the 45-54 years the risk is four times less (up to 5%).
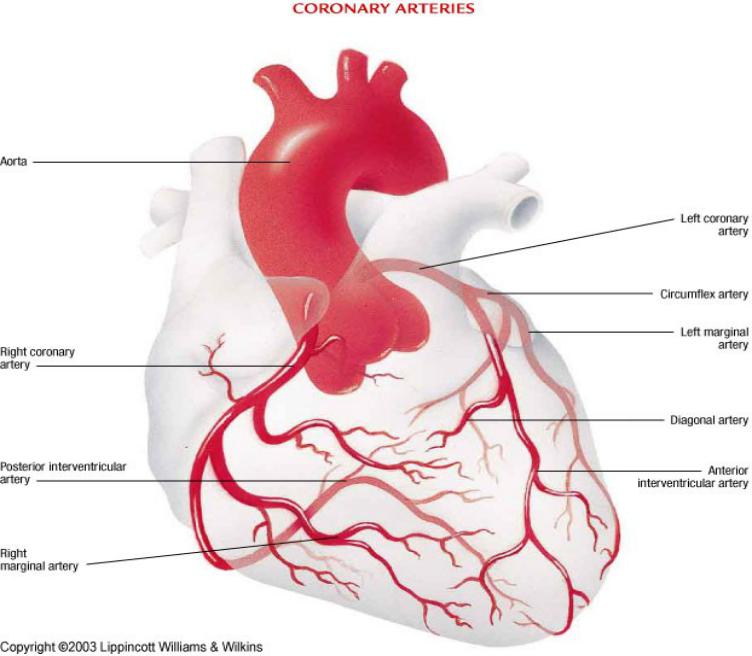
In the normal state, the heart muscle (myocardium) is supplied by the blood vessels with special arteries, which are called coronary or coronary arteries. They leave the aorta and give blood to the myocardium, whose volume normally increases with physical and emotional stress. This allows you to maintain the activity of the myocardium required for a full-fledged activity.
To date, it has been established that the development of angina is directly related to acute violation of coronary circulation. Such a pathology leads to an inadequate supply of oxygen and nutrients to the heart muscle. The result is myocardial ischemia, which contributes to the incorrect flow of oxidative processes. In turn, this leads to the accumulation of various metabolic products in the tissues (phosphorous, pyruvic, carbonic and lactic acids).
Determination of angina of tension by ICD-10 and other classifications
Today, the International Classification of Diseases (ICDs) is the most commonly used in diagnosis. This allows patients to be treated globally if necessary. In relation to stress angina in ICD 10, the following codes are used:
- 120.0 Unstable angina, which includes enlarged angina, the first angst of tension, as well as progressive angina of stress.
- 120.8 Other forms of angina, which include stress angina, stable angina pectoris, coronary syndrome of slow duct.
Classification of angina by definition of WHO from 1979:
- First angina pectoris.
- Progressive angina
- Stable stress angina, which is divided into four functional classes (FC).
Separation of angina in the Soviet classification of coronary heart disease from 1984:
- Angina is stable, which is further divided into functional classes from I to IV.
- The angina is unstable, further separating the Princely Metal angina, postinfarction, progressing and emerging for the first time.

Angina of tension: FC
The determination of the functional class (FC) of angina of stress is based on the general well-being of the patient and his ability to withstand the physical load. Allocate IV FK:
- I FC - normal loads are transmitted to the patient well, whereas at a significant stress an angina attack occurs.
- II FC - restrictions on physical activity are observed. Pain can occur when walking 0.5 km, and it is difficult to ascend the stairs for several spans. Additionally, the risk of angina pectoris increases with the provocative factors (cold weather, emotional tension, sharp wind, activity immediately after awakening).
- III FC - Everyday activities are even more limited. Wine
- There are difficulties during normal walking, when even when moving on a flat surface up to 500 m, the symptoms of an attack are determined. Lifting up the stairs to one floor also causes a deterioration in well-being.
- IV FK - An angina attack can disturb even during insignificant work at home. It is difficult to walk distance up to 100 m. The disease is often manifested in a calm condition.

Symptoms of angina pectoris
In the classic version, the main symptoms of angina are chest pain or discomfort in the sternum . With unstable angina pectoris pain feelings are otherwise characterized:
- more intense;
- last longer;
- progress at lower voltages;
- arise spontaneously in a state of rest;
- arise without any particular reason.
Often in patients with angina pectoris there is any combination of the above clinical manifestations.
A painful attack can be supplemented by other unpleasant symptoms: shortness of breath, lack of air, irregular heart rhythm (arrhythmia), panic, cold sweat.
The angina of the tension is very close to the myocardial infarction. In the case of prolonged intense pain, the appearance of fear of death and abundant perspiration, you should seek immediate medical attention. Also, in such situations, nitroglycerin does not provide the necessary action.

Diagnosis of angina pectoris
To confirm the diagnosis of angina pectoris, first of all, after clarifying the complaints in the patient, the following instrumental studies are conducted:
- Standard ECG
- Definition of heart markers.
- Immediate coronary angiography, which is shown to the patient with complications (for example, persistent chest pain, hypotension, unstable arrhythmias).
With stable patient condition, delayed angiography can be performed, for example, after 24-48 hours .
The assessment starts with a standard ECG and sequential measurement of heart markers. This helps to distinguish unstable angina from acute myocardial infarction (MI), which can occur without elevating the ST segment (NSTEMI) or with the ST segment (STEMI). Such a distinction is the main criterion in deciding on the choice of treatment tactics. For example, fibrinolytics prove to be useful to patients with STEMI, but can be harmed by NSTEMI or unstable angina pectoris. In addition, an urgent catheterization of the heart is indicated for patients with acute STEMI, but is usually not administered under suspicion of NSTEMI or unstable angina pectoris.
- Electrocardiography
ECG is the most important test in the diagnosis of cardiovascular disease. The study should be done within 10 minutes after applying for medical assistance with complaints of chest pain. During an unstable angina, the following changes are determined on the ECG:
- Depression of the ST segment.
- Increase ST segment.
- Tooth inversion T.
The presented indicators are also often transient to the development of myocardial infarction.

- Heart markers
Patients with suspected instable angina pectoris often detect high-sensitivity analysis of cardiac troponin (hs-cTn) immediately after the onset of an attack and after 3 hours.
Cardiac markers are not elevated with unstable angina pectoris. Nevertheless, cardiac troponin, especially when measured using high-sensitivity troponin tests (hs-cTn), may be slightly increased. At the same time, there is no compliance with the criteria for myocardial infarction (above the 99th percentile of the upper control limit).
- Coronary angiography
Patients with unstable angina of the stress whose symptoms have been resolved are usually subjected to angiography within the first 24-48 hours after hospitalization in order to detect injuries requiring treatment. Coronary angiography most often combines a diagnosis with percutaneous coronary intervention (PCI, i.e., angioplasty or stent placement).
After initial evaluation and therapy, coronary angiography can be used in patients with signs of ongoing ischemia (defined by ECG). In addition, the study is used in the presence of hemodynamic instability, recurrent ventricular tachyarrhythmias, and other pathologies that suggest relapse of ischemic events.
Forecast for angina pectoris
The prognosis after an attack of angina of a voltage depends on several components:
- How coronary arteries are affected?
- What arteries are stenotic or obliterated?
- How much blood vessels are struck / blocked?
For example, the proximal left coronary artery stenosis or its analog (proximal left artery and peripheral artery stenosis) have a less favorable prognosis than distal stenosis or stenosis of a small arterial branch.
The function of the left ventricle also strongly influences the prognostic conclusion. In particular, in the presence of significant left ventricular dysfunction (even with a disease of one or two vessels), a lower risk of revascularization of the pathological site is determined, that is, myocardial ischemia will be eliminated by the forces of the body in a shorter time
In general, about 30% of patients with unstable angina tend to have myocardial infarction for 3 months from the onset of the disease . Sudden death occurs in this group of patients less frequently. The marked ECG changes in breast pain indicate a higher risk of subsequent myocardial infarction or sudden death.

Treatment for angina pectoris
Depending on the location of the patient, the treatment of angina pectoris can begin and run in different ways. For example, in the event of an attack at home or at work, the following treatments are performed in turn:
- Durable help.
- Medicinal effect.
- Confirmation of diagnosis using ECG and angiography.
- Reperfusion therapy.
- Post-rehabilitation and long-term medical treatment of coronary heart disease.
Reperfusion is the restoration of blood flow to the organ or parts of the tissue after blockage of the vessel. A similar concept may be related to reperfusion injury and reperfusion therapy.
Durable help
You need to arrange the patient in a calm atmosphere and continue to follow the following sequence of actions:
- Provide oxygen access to the patient.
- Writing to take aspirin or nitrate-containing medicine (nitroglycerin, nitronong forte).
- If you keep the pain on the background of a two-dose medication with a break of 10 minutes, you should contact a doctor or call an ambulance.
Hospital interventions of the medical staff (including ECG control, taking aspirin or nitroglycerin) can reduce the risk of mortality and complications. Early diagnosis and response to treatment often help to determine the need and timing of revascularization.
Video: How to Help Someone with Chest Pains | First Aid Training
Medicinal treatment
Based on the following strategies:
- Assessment of the patient's risk and time reperfusion strategy selection.
- Drug therapy with anti-aggregates, anticoagulants and other drugs based on reperfusion strategy
Upon arrival at the emergency department, the diagnosis of the patient is confirmed by instrumental research methods.Drug therapy and the timing of revascularization depend on the clinical picture. An urgent angiography with revascularization is indicated in the determination of a clinically unstable illness, for example, in the presence of persistent symptoms, hypotension or persistent arrhythmias. In a clinically stable condition, angiography with revascularization can be postponed for 24-48 hours.
Drug therapy for angina pectoris
In most cases, therapy begins with anti-aggregators, anticoagulants, and in the presence of chest pain - antianginal drugs. The choice of drugs used depends on the reperfusion strategy and other factors. Other medications such as beta-blockers, ACE inhibitors and statins may start to be used in the course of ongoing therapy.
In unstable angina, the following drugs are most commonly prescribed (in the absence of contraindications):
- Antiplatelet agents: aspirin, clopidogrel, or both (prazogrel or tacagrelor are an alternative to clopidogrel).
- Anticoagulants : heparin (unfractionated or low molecular weight heparin) or bivalirudin.
- Glycoprotein IIb / IIIa inhibitor , if there is evidence or if there is a high risk.
- Antianginal therapy , expressed in the administration of nitroglycerin in pills or other nitrate-containing drugs in the form of a spray.
- ACE inhibitor .
- Beta blocker .
- Statins
First of all, aspirin is used from 160 to 325 mg (without enteric coating ), if there are no contraindications.Subsequently, for an indefinite period of time, take 81 mg once daily. Chewing the first dose before swallowing speeds up suction.
The use of aspirin reduces the risk of mortality, both immediately after an attack, and in a remote time.

Low molecular weight heparin (LMG), non- fractionated heparin, or bivalirudin are commonly used in unstable angina pectoris if there is no contraindication. In particular, with active bleeding, preparations from this group are not recommended.
- The non-fractionated heparin is more complex in use, since it requires frequent (approximately every 6 hours) dose adjustments to achieve target values.
- LMG has the best bioavailability, the dosage is not so complicated, because it is based on weight, in addition there is no need for titration of the dose. In addition, a lower risk of heparin induced thrombocytopenia is determined.
- Bivalirudin is recommended for patients with known or supposed history of heparin-induced thrombocytopenia.
The glycoprotein IIb / IIIa inhibitor is most often prescribed to patients with a high risk of recurrent ischemia, dynamic ECG changes, or hemodynamic instability. Abciximab, tirofiban and eptifibatide have an equivalent efficacy, therefore the choice of the drug depends on other factors such as cost, availability, acquaintance, etc.
Chest pain can be treated with nitroglycerin , and in extreme cases, morphine . Nitroglycerin is preferable to morphine, which should be used according to certain rules. For example, if the patient has contraindications to nitroglycerin or if he or she has to experience pain, despite the treatment with nitrate-containing drugs, then morphine is used.
- Nitroglycerin is initially put under the tongue (sublingual method of administration), and then, if necessary, is administered continuously intravenously.
- Morphine, administered intravenously, is used every 15 minutes as needed. It is very effective, but it can suppress breathing, reduce myocardial contractility and lead to pronounced venous vasodilation.
Some data also indicate that morphine interacts with some P2Y12 receptor inhibitors. Additionally, information suggests that morphine may increase mortality in a group of patients with acute myocardial infarction. Hypotension and bradycardia can also occur again with the use of morphine, but these complications can usually be overcome by the rapid elevation of the lower extremities.
The standard appointment list for all patients with unstable angina is mainly containing beta-blockers, ACE inhibitors, statins.

Beta-blockers are recommended for high-risk patients, but only if there are no contraindications (eg, bradycardia, heart block, hypotension, or bronchial asthma). Beta-blockers reduce heart rate, arterial pressure and contractility, thereby reducing heart load and oxygen demand.
ACE inhibitors can provide long cardioprotection by improving the function of the endothelium. If the ACE inhibitor is not tolerated due to cough or rash (but not angioedema or renal dysfunction), the angiotensin II receptor blocker is replaced by the drug from another group.
Statins are also standard therapy regardless of the level of lipids, so they should be taken for a long time.

Reperfusion therapy for angina pectoris
Fibrinolytic drugs that may be useful in patients with ST elevation myocardial infarction (STEMI) do not benefit in the case of unstable angina pectoris.
Angiography usually takes place within 24-48 hours after admission to the hospital, especially if the patient has a stable condition. The study is performed with an unstable course of the disease, for example, in case of persistent symptoms, hypotension, stable arrhythmias, etc.
Angiographic data help determine which reperfusion method is best suited.


Rehabilitation and postvaginal treatment of angina pectoris
It is important to change the way of life. In particular, regular exercise, diet change, weight loss, smoking cessation have a positive effect on the state of stressed stenocardia.
According to the medical recommendations after treatment in the hospital, it is often necessary to continue to take antiplatelet agents, beta-blockers, ACE inhibitors and statins.
Больным, которым не проводилась коронарная ангиография при поступлении обычно должны проходить стресс-тестирование до или вскоре после выписки. Единственно, не должны определяться признаки высокого риска (например, сердечная недостаточность, рецидивирующая стенокардия, желудочковая тахикардия или фибрилляция желудочков через 24 часа, а также механические осложнения, такие как новые шумы, шок). Также должна определяться фракция выброса более 40%.
The acute course of the illness and the treatment of unstable angina pectoris should be used to motivate the patient to change the risk factors. Regular evaluation of the physical and emotional state of the patient, if necessary, should be consulted on the way of life (for example, refusal of smoking, organization of a diet, habits concerning work and occupations, physical exercises, etc.). Additionally aggressive risk management can improve predictive judgment.
Key points
- An unstable angina of stress is a new or deteriorating angina of rest in patients whose heart biomarkers do not meet the criteria for myocardial infarction.
- Symptoms of unstable angina pectoris include new or increasing chest pains or discomfort behind the sternum, arising at rest.
- The diagnosis of stress angina is based on the recording of an ECG and the identification of heart markers.
- Immediate treatment for angina pectoris involves the use of oxygen, antianginal drugs, anti-aggregators and anticoagulants.
- Patients with ongoing symptoms, hypotension, or stable arrhythmia necessarily undergo immediate angiography.
- In stable cases, angiography is performed within 24-48 hours after hospitalization and diagnosis.
- After improving the condition, it is important to start or continue to take antiplatelet agents, beta-blockers, ACE inhibitors and statins, as well as those drugs that relate to the underlying disease other than angina pectoris.
Video: Angina: Treatment, causes and symptoms
Similar articles

A pronounced clinic and a long process of development is characterized by angina, formerly known as "chest frog". The disease has specific symptoms that allow faster and accurate diagnosis of the pathology. When performing the patient's medical recommendations, stable angina is characterized by a favorable flow.

Angina is most often manifested by pain in the heart or behind the sternum. At the same time there are additional symptoms indicating a violation of the coronary circulation. When identifying them, it is important to know what to do.

Angina common today is of various forms, but one of the most unfavorable is progressive angina. This disease may be complicated by myocardial infarction, so it is extremely important to know what the disease is.
