ECG decoding
Author Ольга Кияница
2018-10-10

Heart rhythm
Heart rhythm can be regular or irregular.
Irregular rhythms can be:
- Regularly irregular (i.e. the pattern of irregularity is repeated).
- Irregularly irregular (rhythm completely disorganized).
You can distinguish a regular rhythm from an irregular rhythm as follows: Several consecutive RR intervals are noted on a piece of paper. Then the rhythm bars are moved along them to check if the following intervals match.
Nuance of ECG decoding: If there is a suspicion that there is some atrioventricular block, you must specify the rate of contractions of the atria and ventricles (i.e., P-waves and R-waves separately. When movement occurs along the rhythm strip, then you can see whether the PR interval varies.
Similar change can be observed in the absence of the QRS complexes or full dissociation between them. If you additionally measure the RR intervals, then it turns out to find out whether the rhythm is regular or irregular.
Heart axis
The cardiac axis is the general direction of the electrical location of the heart.
In a healthy person, the axis should be sent from 11 o'clock to 5 o'clock (if we evaluate on the dial).
To determine the cardiac axis, you need to look at the standard leads I, II and III.
With a normal cardiac axis:
- II lead has the most positive deviation compared with the leading I and III leads
When deflected to the right:
- Lead III has the most positive deviation, and I lead should be negative.
This change is usually observed in patients with right ventricular hypertrophy.
When the axis deviates to the left:
- I lead has the largest positive deviation.
- Leads II and III are negative.
Left axis deviation is observed in persons with impaired cardiac conduction.
Video: Norm ECG (Russian voice)
Main characteristics and ECG changes
P wave
The following questions are often associated with the analysis of P-waves:
- Are there P-waves?
- If so, is each P-wave accompanied by a QRS complex?
- P-waves look ok? (check duration, direction and form)
- If not, is there any atrial activity, for example, a sawtooth baseline → flutter waves / chaotic baseline → fibrillating waves / flat line → no atrial activity at all?
The nuance of ECG decoding: If P-waves are absent and there is an irregular rhythm, it can trigger atrial fibrillation.
PR interval
PR interval should be between 120 and 200 ms (3-5 small squares)
Prolonged PR interval is more than 0.2 seconds. Its presence may be due to atrioventricular delay (AV-blockade).
First degree heart block
Cardiac blockade of the first degree includes a fixed long interval of PR (more than 200 ms).
Second degree heart block (Mobitz type 1)
If the PR interval slowly increases, then a reset QRS complex occurs, which corresponds to an AV blockade type Mobitz 1.
Second degree heart block (Mobitz type 2)
If the PR interval is fixed, but there is a decrease in the contour, then they say about the AV-blockade type Mobitz 2, and the frequency of the falling blows should be specified, for example, 2: 1, 3: 1, 4: 1.
Third degree heart block (complete heart block)
If the P-waves and QRS complexes are not completely connected, this is the third degree of AV blockade.
Tips for remembering the types of heart block
1. In order to memorize the presented degrees of AV-blockades, it is useful to visually perceive the anatomical location of the block in the cardiac conduction system:
1.1 The first-degree AV-blockade occurs between the sinoatrial node (CA-node) and the AV-node (that is, inside the atrium).
1.2 AV degree second blockade (Mobitz I) is determined at the level of the AV node. This is the only segment of the cardiac conduction system that has the ability to transfer incoming pulses from a higher speed to a lower one. Mobitz II - occurs after the AV node in the bundle of His or Purkinje fibers.
1.3 The third level of the AV block occurs lower in relation to the AV node, which leads to a complete blocking of the conduction of pulses.
Shortened PR interval
If the PR interval is short, it means one of two things:
- The P-wave emanates from a closer region with respect to the AV node, so the conductivity takes less time (the CA node is not in a fixed place, and some of the atria are smaller than others!).
- The atrial impulse gets to the ventricle faster, rather than slowly passing through the atrium wall. This may be an auxiliary path associated with the delta wave. Such an ECG is often observed in patients with Wolff-Parkinson-White syndrome.
QRS complex
There are several characteristics of the QRS complex that need to be assessed:
- Width.
- Height.
- Morphology.
QRS complex width
The width can be described as narrow (NARROW, less than 0.12 seconds) or wide (BROAD, more than 0.12 seconds).
Narrow QRS complex occurs when the impulse is conducted along the bundle of His and Purkinje fibers into the ventricles. This leads to a well-organized synchronous depolarization of the ventricles.
A wide QRS complex occurs when there is an abnormal sequence of depolarization - for example, ventricular ectopia, when the impulse slowly spreads through the myocardium from the focus of excitation in the ventricle. When atrial ectopia is most often determined by a narrow QRS complex, because the impulse passes through the normal cardiac conduction system. Similarly, blockade of branches leads to wide QRS, because the impulse quickly gets into one ventricle through the internal conduction system, and then slowly spreads through the myocardium into the other ventricle.
Height of QRS complex
Described as small (SMALL) and high (TALL).
Small ventricular complexes are determined at a height below 5 mm in the main leads or less than 10 mm in the chest leads.
High QRS complexes most often indicate ventricular hypertrophy (although changes may be associated with a person's constitution, for example, with pain growth). There are many algorithms for measuring ventricular hypertrophy, mainly of the left, among which the Sokolov-Lyon index or the Cornell index is most often used.
Morphology of the QRS complex
During ECG decoding, individual elements of the QRS complex are evaluated.
- Delta wave
The appearance of delta waves is a sign that the ventricles are activated earlier than usual. Early activation with the subsequent slow spread of the pulse along the myocardium causes an indistinct burst of the QRS complex. At the same time, the presence of delta waves does not allow one to unequivocally talk about Wolff-Parkinson-White syndrome. In such cases, tachyarrhythmias combined with delta waves must be identified for confirmation.
- Q-wave
Isolated Q waves can be determined in the normal state. Pathological wave Q is more than 25% of the size of wave R, which follows it, or more than 2 mm in height and more than 40 ms in width. Sometimes it is enough to see the Q waves in various ECG leads to get evidence of a previous myocardial infarction.
Q-waves (V2-V4), with T-wave inversion, may indicate a previous anterior myocardial infarction.
- R and S waves
R-wave is characterized by progression in the chest leads (starting small in V1 and ending in large in V6). The transition from wave S> R to R> S should occur in leads V3 or V4. A bad progression (i.e. S> R to leading V5 and V6) may be a sign of previous MI. Also sometimes determined by people of very large growth due to the location.
- J point segment
The j-point is when the S-wave connects the ST segment. This point can be increased, as a result of which the ST segment that follows it also rises and then speaks of a “high take-off”.
A high take-off (or a benign early repolarization) is a normal ECG variant, which causes many different negative interpretations, since they mainly look at the height of the ST segment.
Important features:
- Benign early repolarization occurs mainly before the age of 50 years (ischemia is more common in people older than 50, which should be suspected first).
- As a rule, the J-point is combined with an increase in ST in many leads, which makes ischemia less likely.
- The T teeth also rise (unlike STEMI, that is, myocardial infarction, when the T wave remains unchanged and the ST segment rises).
- The changes associated with benign repolarization practically do not change over time, unlike myocardial infarction, since during STEMI there will be changes in a week or two or more.
ST segment
The ST segment is the part of the ECG located between the end of wave S and the beginning of wave T. In a healthy person, this segment is comparable to an isoelectric line, which is neither elevated nor decreased. Anomalies of the ST segment are investigated to exclude pathology.
ST segment elevation
The height of ST is considered significant when it exceeds 1 mm (1 small square) in two or more adjacent segments of standard leads or more than 2 mm in two or more chest leads. This is most often associated with acute large-focal myocardial infarction.
Depression of the ST segment
Depression of the ST segment is indicated when there is a decrease of more than 0.5 mm relative to the isoline in two or more adjacent leads, indicating myocardial ischemia.
T tooth
The formation of T waves is associated with repolarization of the ventricles.
T high teeth
T teeth are considered high if they:
- More than 5 mm in standard leads.
- More than 10 mm in the chest leads (the same criteria as in the case of “small” QRS complexes).
High T teeth can be associated with:
- Hyperkalemia.
- Acute myocardial infarction.
Upside down T teeth
T teeth are usually inverted in V1, that is, in the first chest lead, and inversion in standard III lead is a normal option.
Inverted T waves in other leads are non-specific signs of a wide range of diseases:
- Ischemia.
- Purkinje fiber blockade.
- Pulmonary embolus.
- Hypertrophy of the left ventricle (in lateral leads).
- Hypertrophic cardiomyopathy (widespread).
- Generalized pathological process.
When deciphering the ECG, a comment may be added regarding the distribution of the inversion of the T waves, for example. front / side / rear.
Biphasic teeth T
Two-phase T teeth have two peaks and may indicate ischemia and hypokalemia.
Flat prongs t
Another non-specific symptom that may indicate ischemia or electrolyte imbalance.
U tooth
U teeth have a deviation of more than 0.5 mm after T teeth are best defined in the chest leads V2 or V3.
The teeth become larger with slower rhythm (bradycardia). In classical cases, U-waves are determined with various electrolyte imbalances, hypothermia, or antiarrhythmic therapy with drugs such as digoxin, procainamide, or amiodarone.
Key points
- The heart may have a different position in the chest, which depends a lot on the body of a person, the state of the cardiac cavities (their dilatation or hypertrophy), the presence of concomitant pathologies from the pulmonary system, etc.
- V1-V3 can become “right ventricular” if the right ventricle is enlarged, which causes the heart to turn and the right ventricle is in front.
- Severe dilatation of the left ventricle may otherwise be deciphered on an ECG, for example, V5-V6 will show the apex of the heart.
- When deciphering the ECG in different medical institutions, the chest leads may be slightly different, since nurses often install electrodes in different ways.
Video: Norm ECG. All intervals and teeth: p, QRS, T, PR, ST
Similar articles

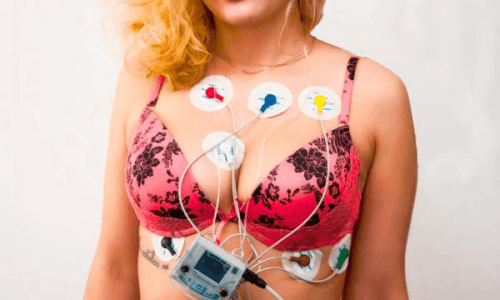
Electrocardiography is the main method for studying the electrical activity of the heart. Many heart diseases are determined precisely by an ECG, which is additionally a relatively affordable way to diagnose. To obtain accurate results, electrodes must be properly applied during ECG recording.
During pregnancy, there are various physiological changes, especially those relating to the cardiovascular system of women. With the help of electrocardiography, some of them can be seen already in the first trimester. To understand whether the pregnancy is normal or there are abnormalities, the decoding of the ECG is carried out.

ECG (or electrocardiogram) is one of the most common and accessible research methods and demonstrates the details of the functioning of the heart in the form of a graphic image that reflects the electrical activity of the organ. This method is often used for the initial diagnosis of cardiac pathologies, is carried out as part of a comprehensive examination of the patient before presumed treatment or during preventive examinations.

Спасибо за полезную статью!Действительно, иногда и не знаешь, как это все понимать…я вот делаю регулярно, таким образом проверяю работу сердца. Мне 50 и хорошо, что все в порядке. Профилактика сказывается. Принимаю курсами двойную омегу-3 от эвалар (именно ее, потому что очень хорошее соотношение цены и качества, да и иммунитет укрепляет к тому же, без чего сейчас никак)+коллаген. Не так все сложно, как кажется…и поддерживать здоровье сердца и себя в целом-вполне посильная задача для каждого.