How are diseases of the gastrointestinal tract and the heart
Author Ольга Кияница
2018-06-29
Disease (from Latin morbus) is a violation of the functioning of individual parts of the body or of the whole organism as a whole. During the disease, homeostasis is disrupted, normal vital activity changes, and sometimes there is a danger to life itself.
A synonym for a disease is a disease, and an antonym is a health.
The disease can be acute and chronic, with various organs and systems of the body being affected. Often the disease is transmitted by heredity, but an important role is played by the way of life that the patient himself leads.Since some diseases develop against the background of other pathological conditions, a combination of GIT and heart disorders is often observed.
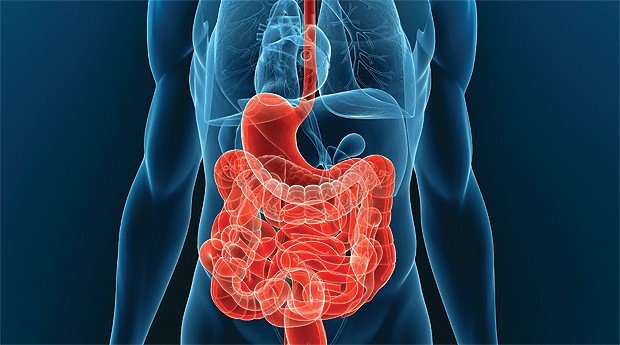
Video: The human digestive system. It's amazing!
Communication of organs and systems in the human body
The human body contains trillions of cells, 78 different organs and almost 100,000 km of blood vessels, if stretched to its full length.
Each organ belongs to one of ten systems of the body, which are interrelated and dependent on each other, which allows them to function in concert. For example, the heart does not beat if the brain and the nervous system do not send signals about it. The skeletal system relies on nutrients derived from the digestive system to create strong healthy bones.
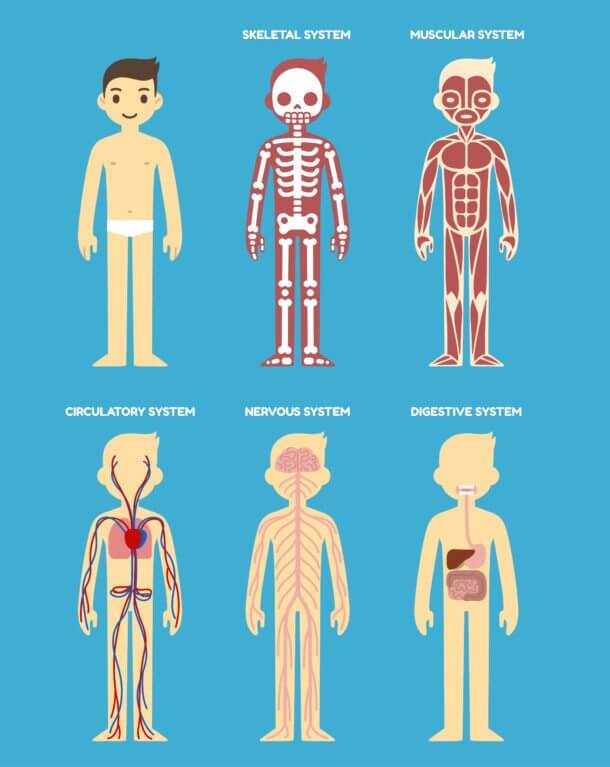
Stylized diagram of the human body's anatomy: skeletal, muscular, cardiovascular, nervous and digestive systems.
There are 10 systems:
- Cardiovascular
- Respiratory
- Nervous
- Muscular
- Skeletal
- Digestive
- Endocrine (hormonal)
- Lymphatic or immune system
- Reproductive
- Cover (leather, hair)
Each body system is a group of parts that work together. The cardiovascular system works for the circulation of blood, while the respiratory system contributes to the intake of oxygen into the body.
Each individual body system interacts with other systems of the body. Blood circulation is a good example of how systems interact with each other. The heart is a pump. When blood circulates through the digestive system, it is saturated with nutrients. Blood also contains oxygen inhaled by the lungs. The circulatory system supplies oxygen and nutrients to other parts of the body, and from there it takes the products of the vital functions of the cells, including carbon dioxide, and transfers these waste to the kidneys and lungs for removal from the body. Also, the circulatory system circulates throughout the body hormones from the endocrine and immune systems.
Each of the systems depends on the normal operation of the rest.
- The respiratory system is based on the circulatory system, which delivers oxygen to all tissues, including cardiomyocytes.
- Bones of the skull and spine protect the brain and spinal cord, but the brain regulates the position of the skeleton, controls the muscles.
- The circulatory system provides the brain with blood and creates the necessary blood pressure, while with the help of nerve impulses, the tone of the vessels and the heart rate are regulated.
Linked, at first glance, unrelated systems. The skeletal system is based on the urinary system to remove metabolic products created with bone cells. In turn, the bones of the skeleton form a skeleton that protects the bladder and other internal organs. The circulatory system delivers oxygen-saturated blood to the bones. Meanwhile, the bones are involved in the creation of new blood cells.
Working together, all body systems maintain internal stability and balance, otherwise known as homeostasis . Disease in one body system can disrupt homeostasis and cause problems in other systems. If, for example, you had to get AIDS, then pneumonia, that is pneumonia, can develop. A yeast infection in the reproductive system, Candida, affects the esophagus and digestive system or causes skin cancer known as Kaposi's sarcoma.
The relationship between gastrointestinal and cardiac diseases
Recently, researchers have scientifically confirmed the connection between the heart and the human digestive system.The obtained data can forever change the way of treatment of patients with heart diseases.
Clinical researchers in Cleveland found that the syndrome of excessive bacterial growth (SIBR, SIBO) is often associated with coronary heart disease (CHD). A study of this issue has allowed to prove that many patients who have one of these health problems had another one.
Patients with SIBO experience a number of side effects, including bloating and abdominal discomfort.
The flora found in the digestive system has always been the focus of researchers, mainly because problems with intestinal health often indicate inflammation elsewhere in the body. However, until now, scientists have not focused on the connection between health of the intestine and heart.

Heart diseases - the leading cause of death worldwide
Heart disease is the leading cause of death both among men and women in the United States and other countries of the world. About 11% of the American population suffers from ischemic heart disease, another 20% of the population determines the growth of small intestinal bacteria.
Researchers still can not say whether SIBO causes SSI or IHD to promote the development of SIBO, but revealing a correlation between them has already proved to be extremely important.
Metabolism can be wrong
Clinical researchers believe that metabolic processes associated with digestion can greatly affect the development of coronary artery disease.
"In fact, we do not know the order of the cause-effect relationships, and this makes the study even more interesting," explains the gastroenterologist Dr. Bo Shen. "We believe that there is a poorly understood connection between the intestines and the heart, in which bi-directional relationships are triggered."
"It is believed that the bacteria of the intestines can cause obesity," added Dr. Shen. "It has been determined that SIBO is more common in patients with morbid obesity, and we do not know if this is the cause or effect."
In addition to obesity, SIBO has also been associated with diabetes and non-alcoholic fatty liver.
Primary gastrointestinal infections and cardiovascular diseases
- Atherosclerosis is a multifactorial disease that develops again against the backdrop of a chronic inflammatory process. Its progression increases with endothelial damage in the early stages to acute coronary syndrome (ACS) due to the instability of plaques and the formation of thrombi as a late complication. The literature indicates that the high incidence of atherosclerosis appears to be the result of both traditional (for example, diabetes mellitus, dyslipidemia) and unconventional risk factors for the type of chronic infections leading to chronic inflammation and disturbance of lipid oxidation.
- Helicobacter pylori - gram-negative bacteria, which, according to statistics, are determined in half of the world's population, are one of the main causes of chronic gastritis and a chronic low-level inflammatory response.Epidemiological studies have shown a correlation between atherosclerosis and H. pylori infection. A specific H. pylori DNA found in atherosclerotic plaques has been detected, which causes an increase in the number of inflammatory markers and lipid profile after H. pylori eradication. It is also assumed that positive strains of H. pylori Cag-A may be more actively involved in the development of coronary artery disease.
Atherosclerosis is also associated with chronic infection with the hepatitis C virus (HCV), which probably develops against a background of chronic inflammation, and is not associated with cholesterol in the patient. In addition, in patients infected with HCV, steatosis of the liver with subsequent metabolic syndrome is more often determined, which aggravates the risk for the cardiovascular system. However, it is confirmed that HCV infection should be considered as an independent risk of cardiovascular disease, regardless of the steatosis of the liver, and the severity of liver fibrosis.
Although some studies failed to reproduce such a correlation, previous studies have shown sequences of HCV RNA with an atheromatous plaque. Much of the literature seems to support the effect of chronic HCV infection on the risk of early atherogenesis, increasing the thickness of intima-media and the development of cardiovascular diseases.
Inflammatory bowel disease and coronary artery disease
As mentioned earlier, chronic inflammation plays an important role in the atherosclerotic process and the stability of plaques, as well as in the predisposition to thrombosis. Inflammatory bowel diseases (IBD) are most often represented by the following pathologies:
- Crohn's disease
- Ulcerative colitis
These pathologies are associated with a chronic inflammatory process, affecting mainly the gastrointestinal tract. Some extraintestinal manifestations have been well studied, but coronary artery disease (ZCA) has a controversial relationship with IBD.
Researchers have suggested a correlation between IBD and PCA due to the presence of several factors. In IBD, the elevated level of homocysteine and CRP, inflammatory markers is classically determined. These components correlate with enhanced oxidation of intimate lipid particles, promoting attachment of inflammatory cells to the endothelium and subsequent plaque formation and destabilization of the vessel wall. In addition, patients with IBD have an increased thickness and stiffness of the intima of the carotid artery, which is a predisposing factor in the development of diseases of the cardiovascular system.
It is well known that the exacerbation of gastrointestinal diseases is associated with venous thromboembolic diseases, and in recent studies there has been a slight increase in the risk of coronary heart disease, especially in women. [1 - Andersen NN, Jess T (2014) Risk of cardiovascular disease in inflammatory bowel disease.World J Gastrointest Pathophysiol 5: 359-365] It was also found that in this population the greatest risk factor is hypertension, whereas smoking, diabetes and Obesity was not clearly identified as a risk factor.
Cirrhosis and cardiomyopathy
The last 20 years it was assumed that heart dysfunction in the presence of cirrhosis is associated with alcoholic cardiomyopathy. But in studies, there was a violation of cardiac function in patients who did not suffer from alcoholic cirrhosis. Since then, there have been numerous reports of systolic and diastolic ventricular dysfunction in patients with cirrhosis, excluding the etiology of liver disease.
Later, the term "cirrhotic cardiomyopathy" (CMM) was introduced, characterized by a decrease in the contractile function of the heart under the influence of stress. Diastolic dysfunction and electrophysiological disturbances are also detected in the absence of a major heart disease. [2 - Yang YY, Lin HC (2012) The heart: pathophysiology and clinical implications of cirrhotic cardiomyopathy.J Chin Med Assoc 75: 619-623]
Most patients with cirrhosis have a normal left ventricular ejection fraction (LVEF) at rest, and subnormal LVEF will only be detected if a physical, pharmacological or pathological disorder occurs. On the other hand, diastolic dysfunction is determined in approximately 50% of patients with cirrhosis. It is characterized by echocardiographic data in the form of a change in transcriptional blood flow with an increase in the work of the atria to fill the ventricle. Conduction abnormalities, especially the long QT interval, are also present in most patients with cirrhosis.
Physiopathological mechanisms of development of MCH:
- Defects of beta-adrenergic receptors
- Membrane Biophysical Changes
- Increased circulation of endogenous substances responsible for hyperdynamic circulation and negative inotropy (for example, nitric oxide, endocannabinoids, carbon monoxide).
Cardiac dysfunction, apparently, contributes to the development of hepatorenal syndrome, which significantly worsens the prognostic conclusion.
There is no special treatment for MTC, so most often follow recommendations for patients with heart failure. Sometimes liver transplantation is the only way of treatment with a proven positive effect. Patients with deteriorated hemodynamic status should undergo an assessment of their condition at the doctor's place of residence. Early recognition of systolic or diastolic dysfunction can help prevent heart failure.
Metabolic diseases of the liver and cardiovascular disorders
Hereditary hemochromatosis is a genetic disorder, which is based on a violation of iron metabolism due to its excessive absorption in the intestine. This leads to supersaturation of the body with iron. There are four types of hemochromatosis, and classical clinical manifestations include:
- Cirrhosis
- Bronze skin
- Diabetes mellitus in the fourth or fifth decade of life.
It is known that the level of cardiac overload with iron is directly related to cardiac dysfunction and death. Initially, precipitation of iron leads to restrictive cardiac dysfunction and, if left untreated, it accelerates left ventricular remodeling followed by the formation of enlarged cardiomyopathy with a reduced left ventricular ejection fraction. Some patients do not develop advanced cardiomyopathy, but diastolic dysfunction leads to pulmonary hypertension and dilatation of the right ventricle without remodeling the left.
Although the deposition of iron occurs mainly in the myocardium, it can also affect the conduction system, which leads to arrhythmias. Cardiomyopathy from iron overload is the result of direct effects on the heart and indirect effects of other dysfunctional organs (eg, liver cirrhosis). Thus, therapeutic phlebotomy should be used to prevent organ damage due to gland over-saturation in all four types of hemochromatosis.
Wilson's disease is an autosomal recessive disorder that leads to the accumulation of copper in certain tissues due to impaired hepatic enzyme ATP7B function. The disease usually manifests itself with hepatic and neuropsychiatric symptoms, although concentrated left ventricular remodeling, enlarged cardiomyopathy and supraventricular arrhythmias can also occur.
Hepatic inflammation with liver biopsy, which may or may not be present with non-alcoholic fatty liver disease (BDT), is called non-alcoholic steatohepatitis (BSH). It is characterized by metabolic syndrome and insulin resistance as the main etiologic factor. BRD is defined in 20-30% of the world population, and steatohepatitis is the leading cause of chronic diseases in the United States and one of the main causes of hepatocellular carcinoma all over the world. The relationship between BRD and cardiovascular diseases depends on their similar risk factors. In some cases, cardiovascular diseases are caused by a metabolic syndrome, and in others cardiovascular pathologies lead to AIV.These factors are difficult to distinguish, since lifestyle, diet and socioeconomic factors lead to both cardiovascular diseases and to the BRD.
Obviously, the presence of BRD leads to an increased risk of cardiovascular disease in diabetics and transplantation, and studies with risk markers such as carotid artery thickness and coronary calcification with computed tomography indicate an increased cardiovascular risk in patients with BSG. There is also evidence that markers of endothelial damage such as sICAM-1, sVCAM-1 and Eselectin have been raised in patients with BRD. [3 - Alvares-da-Silva MR, de Oliveira CP, Stefano JT, Barbeiro HV, Barbeiro D1, et al. (2014) Pro-atherosclerotic markers and cardiovascular risk factors one year after liver transplantation.World J Gastroenterol 20: 8667-8673]
More recent studies have shown that the histology of the liver does not determine the risk of cardiovascular disease.The American Association of Cardiologists studied selected patients with metabolic syndrome and BRD with elevated liver enzymes, who were prescribed lifestyle changes (diet and exercise) and treatment of metabolic syndrome (atorvastatin for dyslipidemia, metformin with glucose intolerance, antihypertensive drugs, orlistat for obesity).
Thus, cardiovascular complications in gastrointestinal diseases are more common than previously thought. Their clinical presentation takes on increasing importance, so with proper treatment it is possible to significantly improve the patient's condition and prognostic conclusion.
Video: Diseases of the gastrointestinal tract. Treatment of diseases of the gastrointestinal tract
Similar articles
Rhythm disturbances are often associated with various diseases of the gastrointestinal tract, which in such cases act as a primary disease. Research in this direction has been going on for many years and today there is a clear link between GI disorders like GERD and cardiovascular system.

A person can use not only a dozen years for the food he likes and at the same time not to know about her harm or benefit to the heart. If the diseases of the cardiovascular system have been determined, then first of all, you should pay attention to your diet. Otherwise, even medical treatment will not be as effective as consuming all the same harmful foods.

In some people, a heartbeat occurs immediately or after a meal. There are reasons for this and if the unpleasant condition does not pass for a long time or if its progression is observed, treatment is necessarily carried out. Necessary recommendations for therapy are given by a cardiologist or a family medicine doctor.
