Arrhythmia with inflammation of the pancreas
Author Ольга Кияница
2018-06-29
Arrhythmia is an upset of the heart rhythm, which should normally be regular, orderly and correct. Changing the activity of the heart does not always have clinical severity, although in other cases the symptoms can reach life-threatening.
Arrhythmia can be expressed in the form of tachycardia (accelerated heartbeat), bradycardia (delayed heartbeat), extrasitolia (extraordinary contractions), paroxysmal palpitation (paroxysmal tachycardia), or blockade.
To clarify the form of arrhythmia and determine the main cause of the disease using a variety of research methods. First of all - electrocardiography, and if necessary, echocardiography, Holter monitoring, roentgenography of WGCs, etc. In the inflammation of the pancreas, various laboratory tests are often carried out.
Video: Pancreatic inflammation: symptoms, treatment, drugs
Description of pancreatitis
In the human body, all systems are closely interrelated, so the damage or frustration of one activity contributes to the dysfunction of the other. In pancreatitis, rhythm disturbances are often observed as an arrhythmia.
Pancreatitis is a disease of the pancreas (inflammation) of an inflammatory nature, which can occur chronically or in an acute form.
Acute pancreatitis (OP) is an emergency that requires rapid medical intervention. If in such cases, medical assistance is provided on time, then the attack goes away and the person returns to his usual life.
Chronic pancreatitis (CP) is a long-lasting pathology, in which symptoms may not be very pronounced. Since they still bother the patient, even if from time to time, this in some cases can disrupt the normal way of life. In addition, the disease often progresses, so after some time, there may be some complications.
Arrhythmia can occur in both chronic and acute inflammation of the prostate. For the latter form of the disease is more typical tachycardia, extrasystole. In chronic pancreatitis, multiple arrhythmias can be defined, including bradycardia and blockade.

The mechanism of arrhythmia in pancreatitis
All internal organs, including the heart and pancreas, are innervated by the autonomic nervous system. To control the work of these two organs, the sympathetic department and the vagus nerve, related to the parasympathetic department of the nervous system, are involved.
The influence of the vegetative nervous system on the pancreas is as follows:
- The wandering nerve is involved mainly in the excretory work of the organ.
- Sympathetic nerve fibers regulate the tone of blood vessels that supply blood to the pancreas.
During inflammation of the prostate, the parenchyma of the organ often swells, may increase in size. This leads to a violation of the outflow of blood, often painful. Such changes affect the functioning of the autonomic nervous system, which reflexively affects the activity of the heart. Also, with pancreatitis, the body temperature often rises and then the heart rate increases by 10 bpm for each degree. As a result, the patient may have a pulse of 120 beats / min or more, indicating a tachycardia.
When inflammation of the pancreas often develops hyperkalemia, characterized by an increase in the amount of potassium in the blood serum.
If a patient other than pancreatitis previously had other cardiovascular diseases, then against the background of an exacerbation of one pathology, another complication develops. Therefore, in such cases, other more unfavorable types of arrhythmia can be determined - atrial fibrillation, ventricular extrasystole, etc.
Causes
When arrhythmia occurs against the background of inflammation of the pancreas, the causes of the underlying disease must be clarified. This will allow, after their elimination, to quickly improve the patient's condition.
The most common causes of pancreatitis include the following:
- Gallstones blocking the digestive tract
- Alcohol abuse, which can lead to the overlapping of small pancreatic ducts
Other possible causes of pancreatitis include the following:
- Injuries to the abdominal organs, including the pancreas
- Complications after surgery
- Renal insufficiency
- Systemic lupus erythematosus
- Infectious diseases like mumps, hepatitis A / B, salmonellosis, etc.
- Cystic fibrosis
- Tumor processes
- Poisoning with poisons and chemicals
For arrhythmia in inflammation of the pancreas, the main cause is pancreatitis. If this pathology is eliminated, the cardiac rhythm can be normalized as quickly as possible.
Symptoms
The following are the most common signs of pancreatitis. However, in each case, the clinical picture can manifest itself in different ways. Symptoms of inflammation of the pancreas most often include:
- Pain in the abdomen , which can be transmitted to the back or chest - this symptom occurs with pancreatitis most often, but it is precisely with its presence that diagnosis is difficult, because then doctors suspect not only arrhythmia, but also myocardial infarction.
- Nausea
- Vomiting
- Increased heart rate - this is just the manifestation of tachycardia, a form of arrhythmia
- Fever
- Diarrhea
- Edema in the upper abdomen
- Ascites, that is, the accumulation of fluid in the abdominal cavity
- Reduction of blood pressure
- Mild jaundice, yellowing of the skin and eyes can also occur
A rapid heartbeat is often accompanied by an increase in blood pressure, which can then decrease with pancreatitis, with the appearance of a clinic characteristic of hypotension.
Severe abdominal pain in the upper abdomen is usually a symptom of acute pancreatitis. Manifestations of pancreatic inflammation can be similar to other inflammatory diseases or pathological conditions. Always need to consult a doctor about the diagnosis.
Diagnostics
The relationship of arrhythmia to pancreatic inflammation can be confirmed or, conversely, disproved if appropriate research methods are carried out. First of all, the doctor studies the patient's medical history and carries out his objective examination.
- In acute pancreatitis, high sensitivity of the abdomen in certain areas and diagnostic points will be immediately identified (Desjardins symptom, Kacha symptom, Shoffar symptom, Mussi-Georgievsky symptom, Mayo-Robson symptom).
- In chronic pancreatitis, the symptom of Tuzhilin is determined, and the patient himself indicates that a diagnosis of pancreatic inflammation has already been made. It is important to clarify how long the disease lasts and how the attacks previously took place.
In the future, depending on the indications, the following studies can be assigned:
- Ultrasound of the pancreas and heart - allows you to assess the structure of organs, their size, functionality. The method is painless and it takes 10-15 minutes to complete it.
- Retrograde cholangiopancreatography , which is performed with the participation of an endoscope. This study is narrowly focused, it helps determine the condition of the pancreas, gallbladder and liver. The method is invasive, so not all fit. In addition, during the study, a contrast agent is used, to which there are contraindications.
- Computer tomography - allows you to get visual images of various internal organs, including the heart and pancreas. The method is based on the use of X-rays and computer software, as a result of which it is possible to obtain detailed images of the required parts of the body.
- Magnetic resonance cholangiopancreatography - with the use of a special contrast agent administered intravenously, the bile ducts and the pancreas are stained, which allows one to assess the condition of the organ.
- Electrocardiography - is performed to assess the electrical activity of the heart, so first of all it is used in the diagnosis of arrhythmia. Additionally shows signs of damage to the heart muscle.
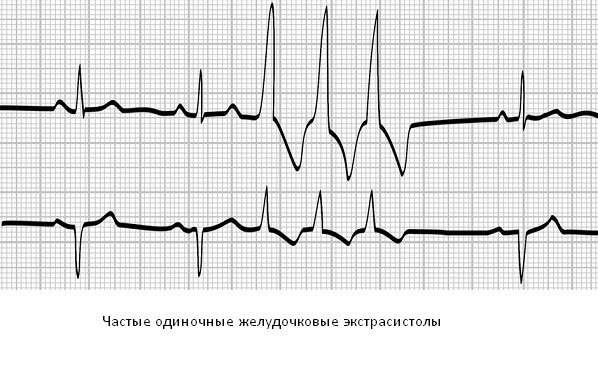
- Holter monitoring - like the previous method of investigation, is used to diagnose arrhythmias that can not be determined by a standard ECG.
If necessary, laboratory tests are performed to assess the extracretory function of the pancreas and the presence of an inflammatory reaction in the body.
Treatment
In order to eliminate arrhythmias in inflammation of the pancreas, appropriate treatment of pancreatitis is necessary, which is determined by the doctor, taking into account the following selection criteria:
- Age, general health and medical history of the patient
- Disease severity
- Tolerance to specific medicines, procedures or anti-inflammatory therapy
- Subjective preferences of the patient.
The overall goal of treating pancreatitis is to allow the pancreas to "rest" and recover from the effects of the harmful factors that caused the inflammatory process.
Treatment of pancreatitis may include:
- Hospitalization for the purpose of observation in hospital conditions and intravenous administration of the necessary drugs
- Surgical effects
- Antibiotic therapy
- Cessation of alcohol use (if pancreatitis is caused by abuse of alcoholic beverages)
- Pain control
- Frequent blood tests (for monitoring electrolytes and kidney function)
- Feeding through the probe for several days
- Placement of a nasogastric tube to feed the patient (a special probe inserted into the nose and guided through the esophagus into the stomach)
Patients with chronic pancreatitis may also require treatment using:
- Enzyme additives to facilitate the digestive process
- Insulin therapy (if the patient is diagnosed with diabetes mellitus)
- Medicines (eg, H2-blockers) to reduce the production of gastric juice in the stomach.
Acute pancreatitis is self-resolving, which means that it usually goes away by itself over time and with the creation of favorable conditions for recovery. Up to 90% of patients recover after acute pancreatitis without any complications.Chronic pancreatitis can also be self-healing, but sometimes there comes an improvement after several attacks. In the chronic course of the disease, a greater risk of developing long-term complications, such as diabetes mellitus, chronic pain, diarrhea, ascites, biliary cirrhosis, bile duct obstruction or pancreatic cancer.
Prevention
The best way to prevent the development of arrhythmia with inflammation of the prostate is to prevent the emergence of the underlying disease. To do this, you need to think in advance about the state of the digestive organs, in particular, it is important to adhere to the following recommendations:
- It is necessary to limit the consumption of alcohol . If you do not consume alcoholic beverages or at least reduce their consumed amount, you can protect the pancreas from the toxic effects of alcohol and reduce the likelihood of developing pancreatitis. In some studies, including in Denmark, involving 17,905 people, alcohol use has been found to increase the risk of pancreatitis in both men and women.
- You should eat low-fat food . Gallstones involved in the development of acute pancreatitis can be formed when excessive amounts of cholesterol are accumulated in the bile. This substance, produced by the liver, takes a direct part in the digestion of fatty foods. Therefore, in order to prevent OP is recommended to eat less fried and fat, and more - whole grains and suitable fruit-vegetables in fresh or cooked form. It is also desirable to moderate consumption of dairy products.
- It is necessary to train regularly and maintain normal weight . People with extra pounds often suffer from cholelithiasis, which greatly increases the risk of developing acute inflammation of the pancreas. The gradual loss of extra pounds, with the maintenance of a healthy weight against a balanced diet and regular exercise, can prevent the formation of gallstones.
- It is important not to practice unsuitable diets , while weight loss should occur gradually. If the patient uses diet food with a very fast weight loss, then the liver activates the process of producing cholesterol, which in turn promotes the formation of gallstones.
- You can not smoke . As research shows, smoking has a direct connection with acute pancreatitis. During the study in Sweden, an assessment was made of more than 84,000 clinically healthy women and men over the age of 46 years. As a result, it was possible to find out that smoking has an impact on the development of OP. The results of the experiments are published in the journal Gut. According to them, people who smoke one pack of cigarettes a day or more for 20 years, are almost twice as likely to develop OP, which is not associated with gallstones. The comparison was conducted with non-smokers. Quitting smoking reduces the risk of a disease that is approaching the same level as that of non-smokers.
Pancreatitis can be quite difficult, and if the necessary measures are not taken, it can cause serious complications.Therefore, if a person is at risk for pancreatitis, then it is necessary to change the daily life accordingly, in order to prevent the appearance of the disease in the future.
Video: Pancreatitis: treatment + diet. Effective treatment of the pancreas without drugs or drugs.
Similar articles
After setting the exact diagnosis, the drugs are prescribed from the existing four classes today: blockers of calcium, potassium and sodium channels, beta-blockers. Also, auxiliary treatment, which includes dietary meals, physiotherapy procedures, moderate physical activity, micronutrient reception, and folk remedies are prescribed. It is important to give up bad habits and, first of all, to cure the underlying disease, that is vegetososudistyu dystonia. The appointment letter must be corrected by the cardiologist, neurologist and, if necessary, the psychotherapist or psychologist.

In the human body, everything is interconnected, so one disease often contributes to the development of another. If necessary, during treatment all the patient's pathologies, including the gastrointestinal tract and the heart, are taken into account. Sometimes an improvement in the course of the underlying disease makes it possible to reduce the clinical signs of another.

The effect of the pancreas on the heart can be called indirect, since there is no direct effect, but in the disorder of the organ's functionality the entire body, including the cardiovascular system, suffers. Pancreatitis pains have a special effect, as they often cause reflex changes in the rhythm of the heart

Связь панкреатита и приступов аритмии не раскрыта. Оформлена в виде “все органы связаны между собой”. Сколько ещё лет ждать? Хоть какой-то проблеск в мед кругах будет в ближайшие лет 10?