Acquired heart defects in children
Author arrhythmia
2019-04-23
Acquired heart defects can occur in children who have been treated for congenital heart defects. These children may be at increased risk of endocarditis, infections of the mucous membrane of the heart or valves caused by bacteria. Acquired cardiomyopathy, that is, an abnormally enlarged or thickened heart, may also develop. In some cases, irregular heartbeats, called arrhythmias, are determined in children and young people.
The procedures or operations used to treat acquired heart defects in children are similar to those used to treat congenital heart defects.
If a child has signs or symptoms of acquired heart disease, a pediatric cardiologist will most likely recommend either echocardiography or magnetic resonance imaging of the heart (MRI). After clarification of the patient's condition, appropriate treatment is prescribed.
Video: Aquired heart diseases in children
The work of the heart is normal and with vices
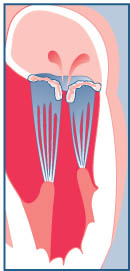
The heart has four valves - tricuspid, pulmonary, mitral and aortic. They have tissue flaps that open and close with contractions of the heart. When opened, they allow blood to flow in one direction through the four chambers of the heart and reach all parts of the body.
With age, there may be two main problems in heart valves: regurgitation, or reverse blood flow, and stenosis.
- Regurgitation occurs when the flaps do not close completely and blood flows back through the valves. This causes the heart to work harder to pump enough blood and satisfy the body's metabolic needs.
- In stenosis, the valves stick together, fuse together due to deposits of cholesterol and calcium on their valves. They cannot fully open, so less blood flows through them.
Since the valve is constricted, the blood has problems passing or leaving the heart chambers. For example, in aortic valve stenosis, blood cannot move from the left ventricle into the aorta. The heart must work harder and eventually weakens, with the result that the left ventricle enlarges and eventually stops functioning normally. This affects the blood flow returning from the lungs, and patients experience shortness of breath from the accumulation of water in their lungs.
In mitral regurgitation (the mitral valve is located between the left upper and lower chambers), the left ventricle must work harder to cope with the blood flowing out. As a result of difficult work, the heart also weakens, and the myocardium thickens. In the end, it can go to heart failure.
The main difference between congenital and acquired heart defects
Not all heart diseases are the same, and there are huge differences between congenital heart defects and acquired heart defects. There is information you need to know about these various heart diseases.
Congenital heart defects (CHD) are determined immediately after birth. These defects are due to structural disorders in the development of the heart at the stage of embryogenesis. There are many stages that the body makes, turning the heart into an organ, and if the smallest part is not formed as it should, it can lead to congenital heart disease. There are no two identical cases of congenital heart disease, and there are specific genetic syndromes with a higher probability of having a defect, such as trisomy 21.
Acquired heart defects (PPS) - a violation that a person acquires in the process of life. In other words, heart problems develop after childbirth, and not during embryogenesis. These are the disorders that most people think about when they imagine that they have “heart problems”. PPP is most commonly seen in older people.
Heart attacks, angina, and excessive calcium buildup in heart valves are the most common types of heart disease in adults. Acquired heart defects, as a rule, are rarely found in children, because their development requires many years.Although rheumatic carditis (acquired heart damage associated with streptococcal infection) is quite common in developing countries. Kawasaki disease is one of the most common causes of acquired childhood heart disease in developed countries.

Differences in signs of congenital and acquired heart defects
Symptoms of congenital heart disease are usually detected very early in a child’s life and can even be detected prenatally (in utero). If a child has a low oxygen level as a result of screening for a pulse or abnormal heart sounds (for example, noise), there is a high probability that he may have a heart defect.
Other symptoms of CHD are considered:
- Poor feeding ability.
- Slow weight gain.
- Change in skin color from head to toe.
Signs of acquired heart defects are much less frequently identified. This disease is more subtle in the sense that it can mimic other infections or diseases. For example, rheumatic carditis is usually diagnosed after a child has had acute pharyngitis. Also, Kawasaki disease is diagnosed at least after five days of fever and after excluding other causes. Often children with PPS have a lower tolerance to physical activity.
Video: Acquired heart diseases in children
Causes of acquired heart disease
Acquired heart defects can result from an infection, such as infective endocarditis and rheumatism. Pathology can also be caused by changes in the valve structure, such as stretching or tearing of the tendons of the chord or papillary muscles, fibro-calcified degeneration or expansion of the annular space of the valve. Sometimes the cause of the acquired valve disease remains unknown.
- Rheumatic fever
Rheumatic fever causes a common type of valve disease. With this acquired heart disease:
- The valves of the heart valve can be inflamed.
- Sash can stick together and become hard, thickened and shortened, and scars are also often formed.
- One or several valves (most often the mitral valve) can become stenotic (narrowed) or valve insufficiency occurs.
Rheumatic fever is usually the result of an untreated streptococcal infection, and is especially common after acute pharyngitis. Using penicillin to treat a sore throat can prevent this disease. Rheumatism is most common in children between the ages of five and fifteen. Sometimes it takes years to develop symptoms of valve disease. The valve itself is not infectious for rheumatism. Instead, the body produces antibodies to fight the infection, and they respond to heart valves, causing them to become inflamed and cause scarring.
- Endocarditis
Infective endocarditis (also called bacterial endocarditis) is a life threatening infection of the heart valves or the lining of the heart (endocardium). It occurs when microbes (especially bacteria, but sometimes fungi and other microorganisms) enter the bloodstream and attach themselves to the surface of the heart valves. With endocarditis:
- Microbes attack the heart valve, contributing to the formation of growths, holes or scars on it.
- Valve insufficiency may occur or stenosis (narrowing) develops.
Microbes can enter the bloodstream during:
- Dental procedures.
- Surgical intervention.
- Intravenous (iv) drug administration.
- The development of severe infections.
If the child already has a valve disease (a mild form of mitral valve prolapse) or had surgery on the valve, then he is determined by an increased risk of developing this disease. Endocarditis can be fatal if left untreated.
Common causes of acquired heart defects, more often defined in adults than in children:
- Coronary heart disease.
- Heart attacks.
- Cardiomyopathy (heart muscle disease).
- Syphilis.
- Hypertension.
- Aortic aneurysm.
- Diseases of the connective tissue.
- Less common tumor diseases.

In some cases, the cause of PPP may be some types of drugs or radioactive radiation.
- Kawasaki disease
Kawasaki disease usually, but not always, affects children under the age of five. This can damage the heart muscle or coronary arteries. The disease is named after a Japanese pediatrician who first described similar pathological cases.The cause of the disease is unknown, but it is probably caused by an abnormal reaction to the intervention of microorganisms. Kawasaki disease is not contagious, although it can occur in separate groups.
The main symptom of Kawasaki disease is constant fever (more than 38.5 ° C) for five or more days. Usually there is no explicit explanation for fever, and it is most often not eliminated by paracetamol. Other symptoms caused by inflammation of small blood vessels, known as vasculitis.
Clinical manifestations characteristic of Kawasaki syndrome:
And - an injection of a conjunctiva on both eyes.
B - “raspberry / strawberry tongue”, bright red and edematous.
C - erythematous rash in the groin area.
D - reddening of the skin and swelling of the hands.
E - redness of the skin and swelling of the feet.
F - peeling of the skin on the tips of the fingers.
G - erythema and edema at the site of a previous BCG vaccination.
H - peeling of the skin on the perianal folds.

Diagnosis of Kawasaki disease
There is no special test for diagnosing Kawasaki disease. The diagnosis is made by eliminating other possible causes of the onset of symptoms. Diagnosis may require a blood test and an echocardiogram to check the heart for changes in the coronary arteries.
Most children who have Kawasaki disease and are receiving proper treatment will recover completely. Several children may develop heart problems, including damage to the coronary arteries. If treatment is not carried out, about 25% of patients suffer inflammation of the coronary arteries, which supply blood to the heart muscle. This can cause irregularities in the blood vessels and blood supply to the heart muscle.
- Cardiomyopathy
Cardiomyopathy is a disease of the heart muscle. There are three main types of this disease:
- Dilated cardiomyopathy is an extension of one or several heart chambers.
- Hypertrophic cardiomyopathy is a thickening of the heart muscle (myocardium).
- Restrictive cardiomyopathy - the heart muscle becomes more rigid and therefore is hard to contract.
In most cases, cardiomyopathy in children develops for an unknown reason. However, possible factors include:
- Heart valve problems.
- Viral infections that cause myocarditis.
- Family history of cardiomyopathy.
- Genetic disorders, including Noonan syndrome.
Cardiomyopathy can manifest by various symptoms. Some people, including children, do not make any complaints in the early stages of the disease. Approximate symptoms may be:
- Swelling of the arms and legs.
- Edema of the abdomen.
- Dyspnea.
- Fatigue.
- Irregular heart rhythm.
- Dizziness and fainting during physical activity.
Diagnosis of cardiomyopathy
In order to determine cardiomyopathy, it can be prescribed:
- Chest X-ray.
- Electrocardiography.
- Echocardiography.
- Blood tests.
In the extreme case, a cardiac catheterization is performed, which allows, if necessary, to take a myocardial biopsy and conduct a histological examination.
Video: Rheumatic Fever & Heart Disease - Pathology
Structural types of acquired heart diseases in children
Changes in the valve structure can occur due to various influencing factors. These include types of structural valve disease.
- Sprain / rupture of ligaments or papillary muscles
The flaps can bend backwards when the ventricles contract, causing the valve to leak. Mitral valve is most susceptible to this. This may be the result of:
- Infections affecting the heart valve.
- Injuries.

- Mitral valve prolapse
Mitral valve prolapse (PMK) is a type of myxomatous valve disease caused by weakening of the connective tissue in the mitral valve. The condition causes the mitral valve to return to the left atrium when the heart contracts. Valve tissues also become abnormal and lose elasticity, which leads to valve failure.
Normally, the mitral valve closes tightly, allowing blood not to flow back when the ventricle contracts.
PMH affects from 1 to 2% of the population. Men and women have the same chance of developing this disease. The condition is usually not a cause for concern. Only a small percentage of patients with MVP ultimately need surgery. If the prolapse becomes severe or is associated with broken chords or cusps, this can lead to serious leakage and immediate surgical intervention.

- Fibro-calcified degeneration
With fibro-calcified degeneration, the valve orifice narrows. The pathological process most often affects the aortic valve.The flaps of the valve become fibrous (thickened) and calcined (hardened), which contributes to the narrowing of the valve opening. The risk factors for this type of valve disease are as follows:
- Increased age.
- Low body weight.
- High blood pressure.
It is often found in adults over 65, whereas in children it rarely occurs.
- Expansion of the valve annulus
The expansion of the annular space of the valve leads to regurgitation (return) of blood. Expansion can occur when the heart muscle is damaged due to:
- Heart attack (heart muscle injury).
- Cardiomyopathy (weakened heart muscle).
- Hereditary disorders such as Marfan syndrome.
- Heart failure.
- High blood pressure.
- Syphilis.
Inherited heart disease, such as Marfan syndrome, can cause an enlarged aorta. Such a violation prevents the correct closure of the aortic valve, which leads to its failure. It can also occur if the aorta is enlarged for other reasons, such as aneurysm, rheumatological conditions, or high blood pressure.
Treatment of Acquired Heart Diseases
Children with congenital heart disease usually require surgery to have their anatomical problem resolved as quickly as possible. Children with acquired heart defects, depending on what defect they have, can undergo surgical treatment or drug therapy.
“Doctors initially use medications to help the heart. When the disease becomes too severe, open heart surgery can be performed, but there is a risk of heart attack, infection or stroke, and even death. Thus, there must be a balance between the need for treatment and the risks of complications, ”notes Professor Yeo Hung Keong, Senior Consultant, Department of Cardiology, National Cardiology Center of Singapore, Member of the SingHealth group.
Surgical treatment options may be as follows:
- Valve replacement using flaps made from pig or cow tissue.
- Implantation of metal or plastic valves in the heart.
The risk of some types of acquired valvular disease (for example, mitral regurgitation) can be reduced by treating conditions such as diabetes and high blood pressure. It also helps to quit smoking, paying attention to diet and regular exercise. Good dental hygiene can also help, as bad teeth often contribute to the development of infection and damage to the heart valves, resulting in damage to them.
Conclusion
Acquired heart defects in children are rarely diagnosed, since their development often takes quite a lot of time — years, and sometimes decades.
The main causes of PPS in children are rheumatic fever and endocarditis. It also increases the risk of having a heart disease if poor oral hygiene is performed, the child often suffers from infectious diseases or is not doing enough sports.
For the treatment of PPS in children, first of all use drugs. If from their reception there is no result, then resort to surgical intervention. In particular, depending on the indications, valve leaflets can be replaced or an artificial valve can be implanted.
Video: Research collaboration gives hope for future of babies with rare heart defect
