Emergency care in acute cardiac left ventricular failure step by step
Author Ольга Кияница
2019-03-03
Acute left ventricular failure (ALVS) is an emergency condition in which the left ventricle undergoes a disproportionate deformity due to hypertension, coronary heart disease or valvular disease. In such cases, LVEF is considered a complication.
The development of acute left ventricular insufficiency is associated with a high risk of death, in particular, some authors indicate that of 250 patients, 59 died during the first six months, and another 69 within the next two years (Palmer, RS, and White, PD; Clinical significance of cardiac asthma. JAMA 92: 431 (Feb. 9) 1929).
There is often very little time left for assessing the patient’s condition, so not only emergency care is important in acute cardiac left ventricular insufficiency by steps, but also the determination of symptoms of the disease.
Video: Acute Left Ventricular Failure | Assessment & Management | Details
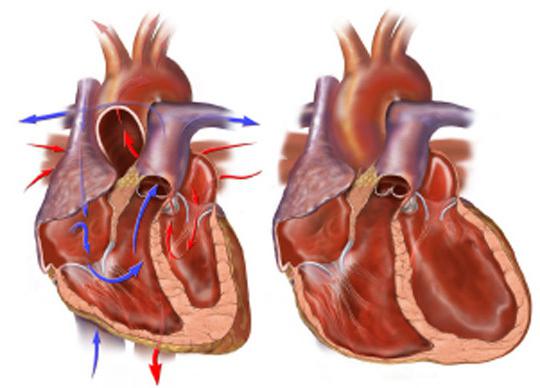
Description of acute left ventricular failure
Acute left ventricular failure manifests as pulmonary edema due to increased pressure in the pulmonary arteries and capillaries. It is important to understand that acute ventricular failure and pulmonary edema are not always synonymous, since
There are other causes of pulmonary edema, such as acute renal failure, acute respiratory distress syndrome (ARDS).
Acute heart failure can be primary (de novo) or develop as a decompensation of chronic heart failure.
Causes of Acute Heart Failure
- Acute myocardial infarction / ischemia.
- Acute mitral regurgitation, which can be caused by:
- rupture of papillary muscle;
- chord break.
- Arrhythmia.
- Aortic dissection.
- Tamponade of the heart.
- Valve failure (eg due to endocarditis)
- Myocarditis.
- Pulmonary edema, for example, against renal artery stenosis, pheochromocytoma.
Typical clinic of acute left ventricular failure
A patient with LBF can detect rapid breathing, often coughing, with the formation of pink foamy sputum. Such signs first indicate the development of pulmonary edema. You may also feel cold and sticky sweat at the periphery due to a violation of peripheral perfusion.
During LLV, as a rule, tachycardia is determined, with increased excitability. Can be heard during auscultation of the heart gallop rhythm (three-membered rhythm). Also, there is widespread crepitus in the chest and
there are wheezing, sometimes even at a distance. When determining low blood pressure (hypotension) they indicate a worsening of prognostic signs.
When determining the first symptoms of acute left ventricular insufficiency, it is important to immediately call a medical team and then provide emergency treatment to the patient.
Video: Pathogenesis of Left Ventricular Failure
Emergency care for acute left ventricular failure
A patient with suspected ALWH should be comfortably seated, after which it will be evaluated using the ABC approach.
- A. It is necessary to check the respiratory tract of a person for patency and increase the oxygen supply. To do this, it can be used to supply oxygen at high speed with the help of special medical equipment such as a traumatic mask. If there are no such devices nearby, then it is advisable to open a window for access of fresh air, especially if the person is in a stuffy room.
- B. It is important to control the patient's breathing and look for signs of stopping. When they appear, urgent resuscitation is needed. Pulsoximetry is also performed when possible.
- C. The patient’s circulatory system is assessed by measuring the pulse and blood pressure. Peripheral blood supply is being examined to check for perfusion. If possible, the patient connects to a heart monitor to detect any arrhythmias. An intravenous catheter is also inserted.
Cardiogenic shock, which is most often caused by acute left ventricular failure, has a very high mortality rate (up to 90%). It is important for the patient to check regularly for signs of shock (severe pallor, fainting, chest pain, feelings of fear).
Video: New Hope for Heart Failure Patients
Medical assistance for acute left ventricular failure
After admission of a patient with OLVD to the hospital, instrumental and laboratory tests are required. Further treatment is prescribed, which allows to improve the general condition of the patient.
Diagnosis of the disease
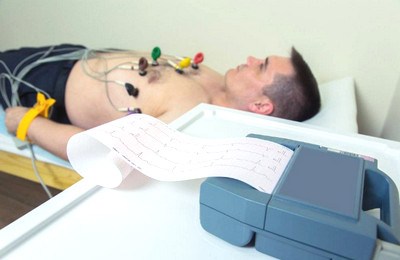
First of all, ECG, blood tests, X-ray examination of OGK, transthoracic ECM are performed.
1 . Electrocardiography (ECG)
Helps determine arrhythmia and ischemic disorders.
2 Blood tests
Complete blood count eliminates anemia as a provoking factor. Additionally, electrolytes are tested (predispose to arrhythmias) and cardiac enzymes (if they can be performed in the hospital). It is worth noting that the level of troponin can often be increased in patients with pulmonary edema, regardless of the cause. An elevated level is not definitive evidence of the development of acute coronary syndrome. This is a fairly useful study, but it is usually delayed until 12 o'clock, and the results are interpreted along with the ECG and other symptoms in a patient.
3. Analysis of the arterial blood gas composition
PO2 is usually low because the alveolar walls are thickened due to fluid, as a result of which diffusion of oxygen through the alveolar capillaries is impaired. PCO2 may be normally low, since carbon diffuses better than oxygen through the alveolar walls, so its excretion is not so susceptible to edema. Elevated pCO2 is a bad sign, as it suggests that the patient’s condition worsens and rapid breathing can no longer be maintained. As a result, the left ventricle cannot deliver enough blood to the tissues, and the blood is poorly filled with oxygen. This means that tissues must switch to anaerobic respiration to meet some of their energy needs, which leads to metabolic acidosis.
4. Chest X-ray
May show diffuse darkening (“shadow of bat wings”) and Curly lines due to interstitial edema and alveolar fluid. The heart most often in acute cases does not increase. Additionally, there may be pleural effusions.
5. Transthoracic ECHO
If a method is available, it allows you to confirm the diagnosis and can help identify the root cause of the disease. This study is considered the gold standard and is conducted by experienced personnel.
Drug management
The initial approach to a patient with acute heart failure is similar to any acute process. There are several principles that regulate the treatment of ALS, and they are based on the pathogenesis of the disease.
The heart is a pump whose function is to maintain the blood pressure at the proper level so that it can flow throughout the entire vascular bed. Flow is the movement of fluid (in this case, blood) from a high pressure area to a lower pressure area. The greater the difference between pressures, the faster the blood moves.
The heart itself cannot dictate how much blood flows into it. It depends on the pressure in the venous system.Nevertheless, a well-functioning heart is able to maintain pressure at a sufficient level in order to pump the volume of blood flowing into its chambers. In heart failure, the heart receives more blood than it can pump, and this leads to an increase in pressure in vessels flowing into the heart and a decrease in blood flow to areas distant from the heart.
As a result, the first principle of treating ALS is to reduce the amount of blood returning to the heart . The blood flows passively from the central veins, through the right atrium to the right ventricle during diastole. The factors that determine how much blood returns to the heart are presented in the form of peripheral venous tone and venous blood volume. Therefore, if the difference between the central venous pressure and the pressure in the right ventricle is reduced, then less blood flows to the right side of the heart and the ventricle has less work. A similar mechanism is also known as preload reduction.
Reducing the amount of blood returning to the heart is achieved by reducing peripheral venous tone, or reducing the volume of venous blood.
- Nitrates are dilators of the venous system and therefore reduce venous tone.
- Furosemide dilates the vessels of the venous system well, and it is this effect that causes the initial relief of symptoms. Due to the diuretic effect, furosemide also reduces blood volume and causes a further decrease in preload. This requires more time for the effect to be noticeable.

The second principle of the treatment of VLVN is about the ptimization of the outflow of blood from the left ventricle. The pressure in the ventricle during systole is created by compressing its walls and pushing the blood contained inside.The pressure in the aorta depends on how much blood enters the vessel (from the heart) and how much blood flows from the other side of the arterial system (through the arterioles to the tissue). The flow rate is directly proportional to the pressure difference, so if there is a big difference between ventricular pressure and aortic pressure, then more blood can flow from the heart. In other words, the stroke volume will increase.
In heart failure, the ventricle cannot maintain a high enough pressure to expel all the blood that remains in its chamber.If the pressure in the aorta decreases, it increases the pressure difference between the ventricle and the aorta and improves heart function.
- Opiates , such as diamorphine and morphine, just increase the pressure difference between the ventricle and the aorta, because they reduce sympathetic activity. The sympathetic system has a number of effects, one of which is to induce vasoconstriction of arterioles. This allows you to hold the blood in the arterial system and raise the pressure in the aorta. A decrease in this sympathetic activity therefore decreases aortic pressure.
- Nitrates , as well as venodilators (dilators of the venous system), are also arterial vasodilators. Therefore, they can help improve outflow from the left ventricle.
The principle of pressure reduction, which the left ventricle must overcome, is known as afterload reduction.
Another way to increase ventricular outflow is to increase the pressure in the ventricle. This is the way inotropic drugs , such as dobutamine, work. There are many serious side effects associated with these drugs, so they can only be used under medical supervision.
The third principle is the treatment of the underlying cause of the LDL . This may be acute coronary syndrome, arrhythmia, or acute lesion of the valve apparatus.
Patients with LVEF need careful observation, so care is usually provided under continuous monitoring conditions - the cardiology department or the intensive care unit. In particular, the work of the heart and respiratory systems is monitored. If necessary, catheterization of the bladder is performed to ensure timely urination.
Today there are advanced methods of treatment of acute left ventricular failure, which are sometimes used in critical cases. In particular, intra-aortic balloon pumps, inotropic drugs and CPAP-therapy can be involved.
Video: Left Ventricular Failure and Cough
