Myocarditis
Author Ольга Кияница
2018-03-04
Myocarditis (MK) is a cardiovascular disease characterized by heart muscle damage due to the development of inflammation in the tissues of the organ. The pathological process is mainly due to the indirect or direct influence of infectious, parasitic, protozoal factors that can be supplemented by chemical and physical effects.
According to WHO data for 1982-1996, a stable heart muscle damage when coxacin Group A virus was infected was developed in 3% of cases, with influenza A in 1.4% of cases, with influenza B - 1.2%, with paragripp - in 1.7% and in adenoviral infections - in 1% of cases.
Clinical and instrumental signs, which are mainly associated with inflammatory heart disease, are important in the diagnosis of the disease. It is also common enough that myocarditis is defined in HIV-infected patients with chlamydia, toxoplasmosis and tick borreliosis. In rare cases, autoimmune myocarditis develops, although the probability of occurrence of MK is much higher with such pathologies as rheumatoid arthritis (up to 25%), systemic scleroderma (up to 40%), systemic lupus erythematosus (up to 15%).
Video: Myocarditis. How not to let colds in the heart
Classification
There are several MK classifications, the most famous of which are the International Classification of Disease Control 10 and the Clinical Classification of 2007. With their help, accurate diagnoses are established, according to which the necessary treatment tactics are selected in the future.
The International Classification of Diseases (ICD-10) includes the following forms of myocarditis:
- Acute rheumatic MK I01.2
- Rheumatic MK I09.0
- Acute MK I40
- Infectious MK I40.0
- Other types of acute MK I40.8
- Acute MK unspecified I40.9
- MK with illnesses from other sections I41
- MK in bacterial diseases from other sections I41.0
- MK for viral illnesses from other sections I41.1
- MK in infectious and parasitic diseases from other sections 141.2
- MK in other diseases from other headings 141.8
- MK unspecified I51 4
The clinical classification of myocarditis in 2007 was developed by Paleyev N.R., Paleyev F.R., Gurevich MA:
- By an etiological factor: infectious and infectious-allergic, immunological and toxic-allergic.
- By the pathogenetic phase of development: infectious-toxic, immuno-allergic, dystrophic, myocardiosclerotic.
- By morphological characteristics: alterative and exudative-proliferative, which in turn can be dystrophic, inflammatory-infiltrative, vascular and mixed.
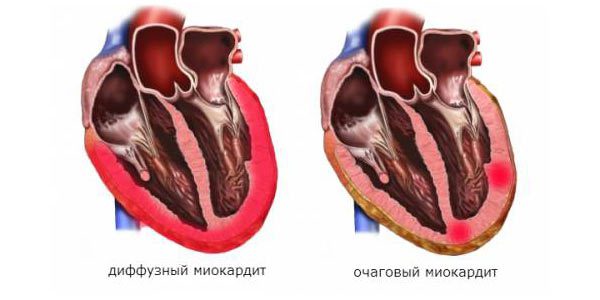
- By prevalence: diffuse and focal.
- According to the clinical course: malosymptomatic, pseudocoronary, pseudoclastic, thromboembolic, arrhythmic, decompensated, mixed.
- In the current: benign, acute, recurrent, with increasing dilatation of the heart cavities and chronic.
In the formation of the diagnosis of ICD-10, as a rule, "acute myocarditis" is indicated with a refinement of the etiological factor of exposure. The microbiological confirmation of the final conclusion must also be indicated. Clinical classification is more often used with the term "chronic myocarditis," which is authorized for use by the WHO Expert Committee in 1997.
Reasons
Over the past 10 years, infectious agents have been studied thoroughly. Various pathogens have been identified, provoking the development of myocarditis, starting with viruses, bacteria, the simplest and ending with fungi, rickettsiae.
Among the numerous pathogens, myocarditis is most commonly caused by viruses. The following arguments support the confirmation of the viral etiology of MK:
- During the period of viral pandemics and epidemics, the number of MKs increases sharply.
- In the course of the examination of patients on MK, viruses are detected in the stools, on the nasal mucous membrane, and, after several weeks from the onset of the development of acute MK in the blood, antiviral antibodies are determined.
- Viral agents are determined in the myocardium, which was inflammatory.
In the course of myocardial development, several pre-determinative factors of development are often isolated. At the same time, one of them helps to activate another. In addition, there are risk factors that increase the likelihood of a disease so to speak "from scratch".
Developmental factors
Myocarditis occurs due to the action of infectious agents on the cardiac muscle, which, due to the introduction of cardiomyocytes, have a direct cytolytic action. Some pathogens carry out myocardial invasion (bacteria, toxoplasma), which can last from several days to two or three weeks. Others secrete toxins (systemic infections like diphtheria and scarlet fever) that damage cardiomyocytes and other cells. Also, systemic immunopathological reactions may lead to non-specific cell damage.
With some diseases associated with drug interactions, changes in serum composition, an antigen-antibody reaction is formed by autoimmune connective tissue injury, which causes the heart to act as the target organ of a large autoimmune reaction. The heart muscle begins to attack the composite units of humoral and cellular immunity, as a result, an inflammatory process with all the ensuing consequences passes through the myocardium.
Some enteroviral-type viruses like Coxacillus B are capable of triggering an immune response in the body, as they are very similar to the cardiomyocyte cell membrane. Therefore, the virus often ceases to exist in the body, while the autoimmune reaction continues to form on target organs.
An inflammatory process that affects the myocardium causes severe structural changes. First of all, inflammatory infiltrates are formed, which include lymphocytes, macrophages, eosinophils, neutrophils. Then the microcirculatory channel begins to overflow with blood, due to which the protective reaction in the form of an arterial spasm works. With the further development of the pathological process, the capillaries and veins undergo paresis, in the vessels the movement of red blood cells stops, fibrin is deposited and microchrombouses arise. If the disease leads to cardiomyocytes to necrosis, then in their place fibrous tissue grows.
A peculiar marker of an earlier developed myocarditis is myocardial cardiosclerosis. It can be diffuse and focal. If together with it is determined inflammatory infiltration and dystrophy of cardiomyocytes, then speak of chronic myocardium.
Risk factors
The main causes of myocarditis can be divided into three large groups:
- Infectious and infectious-toxic - include many different pathogens from the group of viruses (koxa, cyto, arbo, adenovirus, influenza, rubella, measles, chickenpox, infectious mononucleosis, hepatitis B and C, poliomyelitis, AIDS), bacteria (streptococci, meningococci, staphylococci, gonococci, salmonella), spirochete (syphilis, typhoid fever, Lyme disease, leptospirosis), fungi (aspergillosis, candidiasis, coccidiosis, actinomycosis), protozoa (trypanosomiasis, toxoplasmosis, schistosomiasis), parasites (trichinosis), rickettsia (rash typhus fever Ka Ku)
- Immunological (allergic) - MK develops due to physical and chemical factors of influence such as burns, organ transplants, systemic connective tissue diseases, the use of certain drugs, the occurrence of immunopathological reactions.
- Toxic-allergic - the cardiomyocytes are negatively affected by alcohol, narcotic substances, uremia, thyrotoxicosis.
Video: Myocarditis as a consequence of an allergy
Few statistics on the connection of myocarditis with various infectious-toxic effects factors:
- In 50-60% of cases diphtheria patients die from cardiac complications.
- Up to 5% of patients suffer from myocarditis in the epidemic of influenza.
- Chronic infectious diseases can also be complicated by inflammatory heart disease, and the like is detected in an average of 20% of patients.
- The average age of patients with myocarditis is 30-40 years.
- Myocarditis is known to medicine for more than 200 years, but until now, issues related to etiology, disease development, specific treatment, etc. have not been resolved.
Species
In clinical practice, etiologic variants of myocarditis differ, which differ in character, flow, and prognostic significance.Depending on the excitatory factor, appropriate treatment tactics are used. It is worth considering the most common etiologic types of myocarditis.
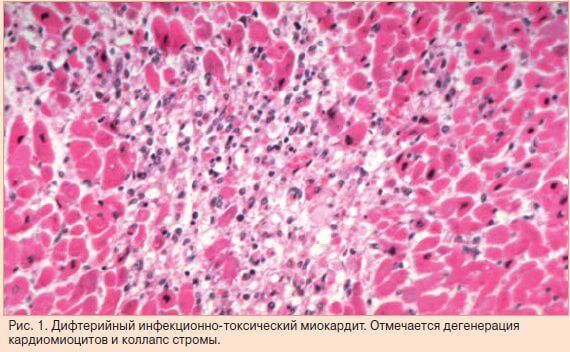
Diphtheria myocarditis
The main disease is complicated by MK in 8% of cases. If the course of the illness is severe, then the risk of myocarditis reaches 50%. This is due to the fact that the diphtheria toxin has a high degree of cardiotoxicity, because of which the heart cells quickly perish and become to the body by foreign agents, which produce an immune response.
Clinic . The current is a severe, rather severe symptom of heart failure (shortness of breath, heart pain, edema).Arrhythmias and heart blockages may occur. The first signs of myocarditis in the background of diphtheria often appear at 8-10 days from the onset of the disease, the more favorable course of the disease is observed with the development of MK in the third to fourth week of the disease.
Salmonella myocarditis
Often accompanied by a hard-running salmonellosis. It is mainly manifested in children, while increasing the risk of death. Salmonella infection can contribute to the formation of abscesses in the myocardium, resulting in the development of a fatal tamponade (stop) of the heart.
Clinic . Symptoms are developing as they grow. At first, pain in the area of the heart and fatigability can occur, but gradually signs of severe heart failure appear, which in severe cases complicates vascular thromboembolism. Yet, in most cases, the clinic MK with salmonellosis is not strongly expressed, which is confirmed by non-specific changes in the ECG.
Septic myocarditis
The modern use of highly active antibiotics allowed to reduce the number of MK arising from the background of sepsis, up to 4% of the total number of myocarditis. When septic MK is most often determined by pseudomonas aeruginosa, staphylococci, coli and other pathogenic flora.
Clinic Sepsis is characterized by a pronounced and severe clinic, which, in the case of myocardial attachment, is accompanied by paroxysmal tachycardia or atrial fibrillation. The patient may have a tachycardia that does not correspond to body temperature, which is usually increased with sepsis. With the further development of the pathological process, heart failure develops.

Viral myocarditis
The most commonly diagnosed among various etiologic forms of myocarditis, which is associated with high cardiotropicity of the Koksaki virus B. The disease can develop at any age, but there is evidence of an increase in the incidence of pathology after 50 years, with men more susceptible to it. Women are at increased risk of developing viral myocarditis during pregnancy or after delivery. In the case of a pregnant MK, there is a possibility of stillbirth or myocardial development both in the fetus and in the first 8 months after birth.
Clinic Together with the characteristic symptoms of myocarditis in the patient, high temperature and gastroenteric syndrome can be detected when nausea, vomiting, pain near the navel and upper abdomen appear. Additionally, inflammation of the testicles, enlargement of the spleen and lymph nodes can be diagnosed. A relationship was found between the severity of the clinical picture of the viral MK from the ages of patients. In 17-20 years, a brighter clinic, with frequent manifestations of pleurisy or pericarditis, is determined, but at the same time it ends with recovery. After 40 years the clinic is less pronounced, there may be cardiac pains taken for attacks of the coronary heart disease. Also, sometimes there is a shortness of breath and a heartbeat.
Diagnostics
In the definition of myocarditis, clinical signs are important. They can be more or less specific, often associated with previously infectious or allergic diseases. The following symptoms that may affect the thought of myocardium also matter:
- Cardialgia is a hallmark of MK. Pain in the region of the heart can be spiky, pressing, boring. It is not stopped by nitroglycerin and its duration is practically constant, unlike IBS.
- Fever - often occurs with MK, but this symptom is not characteristic.
- Disruption of the central and autonomic nervous system, manifested in the form of fatigue, weakness, increased sweating, headache.
- Signs of a violation of the respiratory system in the form of an acoustic voiding voice, difficulty in breathing, runny nose, cough.
- Changing the functioning of the digestive system by type of nausea, vomiting, abdominal pain may also indicate myocarditis.
- Pain in the muscles and joints often indicates an inflammation of the myocardium.
After collecting complaints, the doctor must perform a physical examination, during which signs of right ventricular and left ventricular insufficiency can be detected. Further, palpation and percussion of the heart are performed, auscultation of cardiac activity, but more information can be obtained using instrumental and laboratory methods of research.
Laboratory diagnostics allows to determine the markers of damage and destruction of cardiomyocytes. In particular, with necrosis increases LDH, creatine kinase and cardiac troponin. To detect an etiological cause, an agent is searched for. For this purpose blood, urine is examined, necessary serological reactions are carried out, the appointment of which is taken by the attending physician.
Electrocardiography is mandatory, as it helps to detect changes in the myocardium in almost 90% of patients. Similar ECG signs are not specific, but with their help it is possible to find out the localization of the inflammatory focus. The most frequent ECG signs of myocarditis:
- change in tooth T (occurrence is 70%);
- change of segment ST (occurrence - 50%);
- Extrasystole of ventricular and supraventricular localization (occurrence - 45%).
Video: ECG with myocardium, pericardium and Tela
Echocardiography is performed to evaluate the condition of the heart ventricles. The systolic and diastolic function of the heart is necessarily determined. The contractility of the myocardium will be noticeably impaired in severe myocardial flow, while the asymptomatic and malosymptomatic MK on the ultrasound device is practically not determined.
In order to confirm cardiomegaly, radiography is prescribed. Also, this study can confirm the presence of left ventricular failure, especially in the case of determining the appropriate symptoms.
Depending on the clinical picture, other instrumental methods can be used in the form of scintigraphy, magnetic resonance imaging, ultrasound densitometry of the myocardium, endomyocardial biopsy.
Complications
Asymptomatic and malosymptomatic myocarditis can be well treated, resulting in almost completely cured disease.
Acute myocarditis of severe course is often complicated by arrhythmias and cardiac insufficiency. If the disease is not treated or the therapy is not carried out in full, then the risk of sudden death of the patient increases.
Chronic myocarditis in the course of its development is most often complicated by a sclerotic lesion of the heart.Because of this, time can be diagnosed with myocardial cardiosclerosis.
Treatment
Depends on the stage of development of myocarditis and etiologic cause. There is a definite scheme of treatment for patients with myocarditis:
- First of all, etiotropic drugs are prescribed, groups of antibacterial agents or antiviral drugs are selected.
- Anti-inflammatory drugs are needed to remove tissue swelling, improve local blood supply.
- Antihistamines - reduce the severity of the immune response.
- Anticoagulants - are necessarily prescribed to patients aged after 50 years because of the increased risk of developing thromboembolism.
Diuretics, beta-blockers, ACE inhibitors can be used depending on the indications. The last two groups are shown in the presence of a patient with arrhythmia.
Ending etiotropic therapy does not mean stopping treatment. Most often, it continues due to prescribed antioxidants and vaccine prophylaxis.
The first results of treatment of myocarditis are evaluated after six months, for which a number of studies are conducted to determine changes in the concentration of cardiolective enzymes and the autoimmune reaction. It is important to re-cardio monitoring with the help of ECG and ultrasound of the heart.
Treatment of patients with myocarditis is usually stationary, after which, if necessary, a conclusion is made on the suitability of the patient.
Can myocarditis recur? Yes, and when the symptoms of the disease occur, re-treatment with etiotropic drugs together with metabolic drugs is carried out.
Prevention
First of all, it is represented by a specific vaccine prophylaxis. It is also important to prevent the development of re-myocarditis, for which the etiological, metabolic and other types of treatment must be fully implemented.
During myocardial therapy, it is important to adhere to strict bed rest, which is also considered to be preventative relapse of the disease.
Important measures to prevent myocarditis:
- Reconstitution of chronic foci of infection.
- It is not necessary to communicate closely with patients with viral and bacterial diseases.
- If you have the first symptoms of heart disease, you should contact the cardiologist immediately.
Forecast
Complete recovery is predicted when the patient is asymptomatic or clinically not expressed myocarditis. The severe course of the disease may be complicated, therefore, in such cases, the outlook is worse: 50% of patients recover completely, whereas dilation cardiomyopathy is determined in the rest.
Myocarditis may involve the following risks:
- Sudden death often occurs with the development of arrhythmia against myocarditis.
- Rapid progression of myocarditis often results in heart failure and, as a result, death.
- At giant-cell myocardium Abramova-Fidlera the most unfavorable prognosis is given.
In the development of lymphocytic or giant-cell myocarditis, in most cases, a heart transplant is performed. Otherwise, only 11% of patients with a similar illness survive 4 years or more.
