Atrial fibrillation
Author Ольга Кияница
2018-03-17
Atrial fibrillation (MF) is the most common cardiac arrhythmia. Today, it affects 2.7 to 6.1 million people in the United States. The development of MF in many respects depends on age, therefore, 4% of people are over 60 and 8% over 80 years old. Approximately 25% at the age of 40 years and older is marked by the development of MF throughout life.
The prevalence of atrial fibrillation is 0.1% in persons younger than 55 years old, 3.8% in persons 60 and older, and 10% in persons over 80 years of age. As the number of elderly people worldwide increases, the prevalence of MS can be doubled by 2050.[1 - Abdel Latif A; Messinger-Rapport BJ. Should nursing home residents with atrial fibrillation be anticoagulated ?.Cleve Clin J Med. 2004; 71 (1): 40-4]
In childhood, MF occurs rarely, with the exception of cardiosurgical situations. The incidence of MS is significantly higher in men than in women of all age groups. The disease is more common among white race people than among black people. In spite of this, both cases require careful treatment and prevention of recurrence of arrhythmias.
Video Flicker Arrhythmia - How It Happens
Description
The atrial flicker is an abnormal heart rhythm that occurs when electrical impulses come from different atrial portions (upper chambers of the heart). As a result, the heart begins to work disorganized. This leads to the fact that the atrium is often contracted and an irregular heartbeat or pulse is felt. In severe cases, flickering of the atria leads to stroke development.
Atrial fibrillation often depends on other cardiovascular diseases:
- heart failure;
- coronary artery disease;
- valve heart disease;
- diabetes mellitus;
- hypertension
MS is characterized by irregular and often rapid heart contraction. Exact mechanisms by which cardiovascular risk factors predispose to MS are not fully known, but are under intense research. Redundancy of catecholamine, hemodynamic and metabolic stress, ischemia and atrial fibrillation, activation of the neurohumoral response of the organism often contribute to the development of MF.

A bit of statistics on atrial fibrillation:
- In 10-15% of cases, MF occurs in the absence of concomitant diseases.
- The frequency of ischemic stroke in patients with nonreumatic MP is on average 5% per year.
- The prevalence of stroke in patients younger than 60 years is less than 0.5%; however, in the age of 70, the prevalence rate doubles every decade. [2 - Rathore SS; Berger AK; Weinfurt KP; Schulman KA; Oetgen WJ; Gersh BJ; Solomon AJ. Acute myocardial infarction is complicated by pre-fibrillation in the elderly: prevalence and outcomes. Circulation 2000; 101 (9): 969-74]
- The relative risk of developing stroke with MS is 1.5% for patients aged 50-59 years and is approaching 30% for patients aged 80-89.
- Women are at higher risk of stroke due to MI than men.
Reasons
The atrial flicker is most often associated with the following risk factors:
- Hemodynamic disorders
- Ischemia of the atrium
- Inflammation of the heart of different localization and origin
- Cardiovascular and pulmonary diseases
- Use of alcohol and drugs
- Endocrine disorders
- Neurological disorders
- Hereditary predisposition
- The elderly patient
Hemodynamic disorders
The increased pressure within the atrium leads to its electrical and structural remodeling, which causes the MP. The most common causes of elevated pressure in the atrium are damage to the mitral or tricuspid valve and left ventricular dysfunction. Systemic or pulmonary hypertension also contributes to an overload of the atrium. Much less commonly occur intracardiac tumors or thrombi that change hemodynamics of the heart.
Ischemia of the atrium
Also known as coronary artery disease. May contribute to the development of ischemia of the atrium and ventricles. It is in the second case that most often increases intracardiac pressure, and on the background of this develops MP.
Inflammation of the heart of different localization and origin
Myocarditis and pericarditis can be idiopathic or arise against a background of vascular diseases, connective tissue disorders; viral or bacterial infections. All these disorders can be a cause of MS. Also, cardiac, esophageal or thoracic surgery can provoke the appearance of an MI.
Diseases of the cardiovascular and pulmonary systems
Atrial fibrillation is often associated with:
- Pulmonary embolism
- Pneumonia
- Lung cancer
- Hypothermia
Use of drugs and alcohol
Studies have found that acute or chronic alcohol use (such as festive or Saturday binge drinking) and the use of illicit drugs (that is, stimulants, meth tofetamins, cocaine) are often associated with MS. The connection between more than moderate chronic consumption of alcohol and MP was noted in several studies for a long time. At the same time, recently another study found a connection between moderate consumption of alcohol with an increased risk of developing MS. [3 - McManus DD; Yin X; Gladstone R; Vittinghoff E; Vasan RS; Larson MG; Benjamin EJ; Marcus GM. Alcohol Consumption, Left Atrial Diameter, and Atrial Fibrillation. J Am Heart Assoc. 2016; 5 (9)]
Endocrine disorders
MP can cause hyperthyroidism, diabetes and pheochromocytoma.
Neurological disorders
Intracranial pathologies such as subarachnoid hemorrhage or stroke may contribute to the appearance of MF.
Hereditary predisposition
Transmission of MF due to heredity may be associated with certain anomalies of the ion channel, especially with sodium channels. Also, in some studies, it is assumed that family MS often depends on the increased risk of the disease, which is not fully understood.
Old age
Perhaps, most of all other causes matter the age of the patient. It is known that 4% of persons over the age of 60 years and 8% of people over 80 years of age are defined by the MP.
Video Fibrillation of the atrium, the main causes
Species
- Paroxysmal atrial fibrillation - episodes of MS are observed, which end spontaneously for 7 days (most episodes last less than 24 hours).
- Persistent fibrillation of the atrium - attacks of arrhythmias that last for more than 7 days and may require resection by pharmacological or electrical intervention.
- Long-term persistent flickering of the atrium - the symptoms of the disease persist for more than 12 months either because of a failed cardioversion, or if cardioversion was not timely undertaken.
- Continuous Atrial Flicker - Further strategies for restoring the rhythm have been interrupted after taking common clinical decisions.
This classification scheme is most often used in cases not related to the reversible cause of MS (for example, thyrotoxicosis, acute intoxication with ethanol).
Paroxysmal MT
Atrial fibrillation is considered to be a recurrent pathology when a patient has 2 or more attacks. If the recurrent MP terminates spontaneously, it is called paroxysmal.
It has been found that in some patients with paroxysmal MS, usually younger, there are clear electrically active foci in the pulmonary veins. At the same time, there was a large number of atrial premature impulses marked on the Holter monitor. Isolation or elimination of these foci allows to eliminate trigger activity, which promotes paroxysms of MP.
Paroxysmal MT may progress to a stable form of the disease. In such cases, aggressive attempts to restore and maintain sinus rhythm can contribute to the development of concomitant diseases associated with MF.
Persistent MP
If the recurrence of atrial fibrillation persists, it is considered to be persistent, regardless of whether the arrhythmia is discontinued by pharmacological therapy or electrical cardioversion.
Persistent flickering of the atrium can be either the first sign of the disease, or the result of repeated episodes of paroxysmal MP. Patients with persistent MS also include patients with perennial paroxysms who did not undergo cardioversion or developed a permanent MS after it.
Long-term persistent MP
This form of MS develops for more than 12 months, but there is a decision to restore sinus rhythm. The main goals of the treatment are to control the rate of heart rate and anticoagulation.
Permanent MP
Signs of flickering atrium persist for a long time, more than one year. In this case, cardioversion could be carried out, but in such cases it is often ineffective. Alternatively, cardioversion could not be performed at all.
Clinic
The atrial flicker usually results in the lower chambers of the heart, the ventricles, contracting faster than usual. When this happens, the ventricles can not completely fill with blood. Thus, they do not pump blood sufficiently into the lungs and throughout the body. This can lead to signs and symptoms.
Clinical manifestations of atrial fibrillation cover the entire spectrum from asymptomatic flow to rapid development of cardiogenic shock or cerebrovascular injury.
At atrial fibrillation, the following symptoms are most commonly identified:
- palpitations (feeling of rapid heart rate);
- dizziness or feeling weak;
- frequent urination;
- Shocking breath;
- fatigue;
- shortness of breath
In the asymptomatic course of the disease, the most common symptom is the stroke, which manifests itself as dizziness, severe weakness, "flies" in front of the eyes, numbness in the body.
The clinical picture of the MP according to the EHRA classification is divided into four classes:
- The first one is manifestation
- The second - the usual way of life is not disturbed, although the mild symptoms of the disease are determined.
- The third - the normal life activity is broken due to the expressed signs.
- Fourth - the patient can not perform the usual work because there are signs of disability.
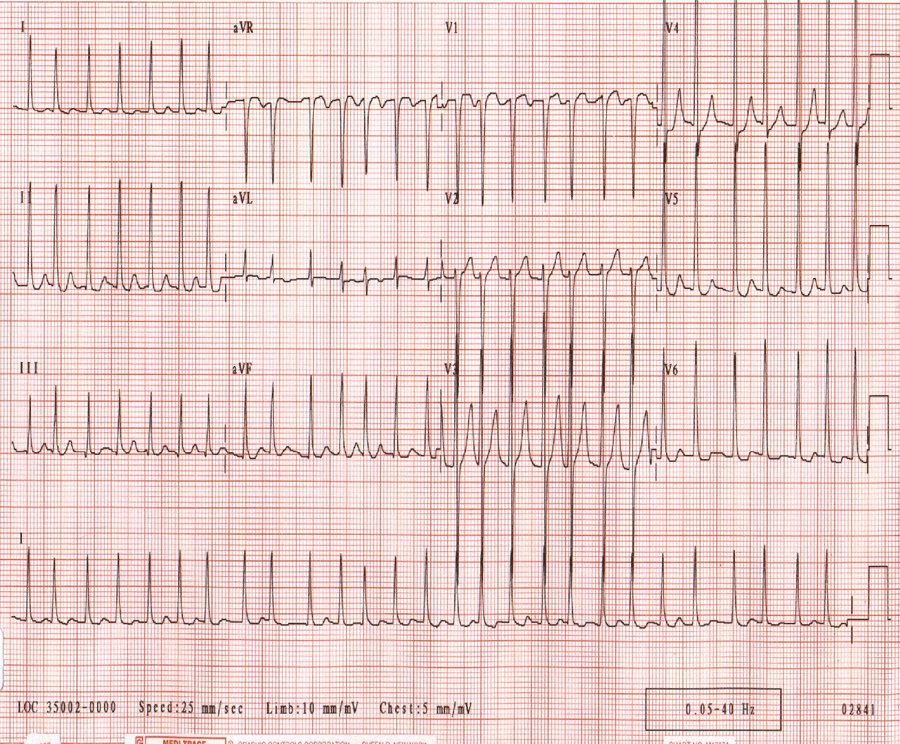
Diagnostics
The analysis of standard electrocardiography (ECG) usually confirms the diagnosis of atrial fibrillation and is based on the following diagnostic criteria:
- Irregular ventricular contractility (QRS complexes) is observed.
- There are no discrete P waves, instead of them there are irregular chaotic F waves
- RR intervals become shorter (Ashman phenomenon)
- The heart rate is increased (usually 110-140 beats / min, rarely 160-170 beats / min)
- Signs of premature agitation
- Left ventricular hypertrophy
- Intraventricular conduction delay
- An acute or pre-existing myocardial infarction
Transthoracic echocardiography (TT echocardiography) is indicated in the following cases:
- An assessment of heart valve damage is necessary
- To find out the size of the atrial and ventricular chambers and their walls
- To determine the function of the ventricles and the presence of blood clots in the ventricles
- In order to calculate the systolic pressure of the lungs, it allows to determine pulmonary hypertension
- Detect Pericardial Disease
Transesophageal echocardiography (TEF echocardiography) is required for:
- Definition of thrombi in the atria (especially in the appendage of the left atrium)
- Carried out cardioversion (if thrombus is detected, cardioversion should be delayed)
Treatment
Atrial fibrillation tactics are based on heart rate control and anticoagulation. Rhythm control is also performed in patients with symptomatic limitation of MF. When choosing treatment tactics, the following criteria are taken into account:
- The severity of the symptoms
- Possibility of preservation of sinus rhythm after successful cardioversion
- The presence of concomitant diseases
Anticoagulation therapy
The American College of Cardiology (ACC) / American Association of Cardiac Diseases (AHA) has developed the following principles for anticoagulation for patients with MS:
- If there are no risk factors then there is no need for anticoagulant or antiplatelet therapy
- The presence of one moderate risk factor is an indication for administration: aspirin at a dose of 81-325 mg / day or anticoagulants
- The presence of any high risk factor or more than one moderate risk factor is an indication for the use of anticoagulants
The risk factors for thromboembolism in MS are as follows:
- High risk factors: pre-existing stroke or transient ischemic attack (TIA), systemic thromboembolism, or age 75 years and older.
- Moderate risk factors: age 65-74, female gender, hypertension, diabetes mellitus, heart failure, arterial disease (preinfarction state, peripheral arterial pathology, aortic plaque).
Anticoagulation therapy is mainly carried out by warfarin. If necessary intravenous heparin and low molecular weight heparin are used. There are also new-generation oral anticoagulants that represent an alternative to heparin. They are most commonly prescribed to patients with non-vascular MP. Their action is almost instantaneous, eliminating the need for binding to heparin.
New oral anticoagulants approved by the US Food and Drug Administration (FDA) include the following:
- One direct inhibitor of thrombin: dubigatran
- Blood Clotting Factor III Inhibitor: rivaroxaban, apixaban, edoxaban.
Risk of bleeding
The choice of suitable antithrombotic therapy is maximally balanced between the risk of stroke and the risk of bleeding. The factors that increase the risk of bleeding with anticoagulants include:
- History of bleeding (the strongest predictive risk factor)
- Age over 75 years old
- Hepatic or renal failure
- Malignant processes in the body
- Thrombocytopenia or the use of aspirin
- High Blood Pressure
- Diabetes mellitus
- Anemia
- Pre-dilation condition
- Genetic predisposition
For patients with clinical anticoagulation indications that have an unacceptably high risk of bleeding, there are two alternatives to treatment:
- Isolation of the left atrium using a catheter-based WATCHMAN device (the only FDA device currently approved in the US)
- Ligation of the left atrial appendage using the LARIAT epicardial / endocardial suture system
Ratings of management strategies:
- Medications: calcium channel blockers (without dihydropyridine), beta-blockers, digoxin, amiodarone (prescribing mainly for patients who do not tolerate or do not respond to other medications)
- Atrioventricular site modification with permanent pacemaker placement (invasive procedure recommended for patients whose other rhythm control options do not help)
Modern rhythm control tactics:
- Electric cardioversion (commonly used as a first-line strategy for young patients with MMP symptoms)
- Drugs (flekainide, propafenone, dopecilid, amiodarone, sotalol)
- Ablation (catheter, surgical or combined)
Immediate cardioversion of the direct current is shown to the patient with the following types of unstable hemodynamics:
- Decompensated Congestive Heart Failure
- Hypotension (low blood pressure)
- Uncontrolled angina / ischemia
Catheter ablation is recommended in the ACC / AHA guidelines from 2014 for the following cases:
- Patients with symptomatic paroxysmal MT, which is susceptible to drugs and methods that control the rhythm.
- For the treatment of patients with symptomatic persistent IB, which can not be cured with the use of appropriate drugs.
- As an alternative to patients with relapsing symptomatic paroxysmal MP who had not previously tried a drug that controls the rhythm.
Complications
Atrial fibrillation has two major complications - stroke and heart failure.
Stroke
During MP, the upper chambers of the heart, the atrium, do not pump the proper volume of blood into the ventricles. Some blood remains in the atria. When this happens, a thrombus may develop.
If a clot falls into the general bloodstream and moves into the brain, it can cause a stroke. (A blood clot that forms in one part of the body and moves with blood flow to another is called embolus).
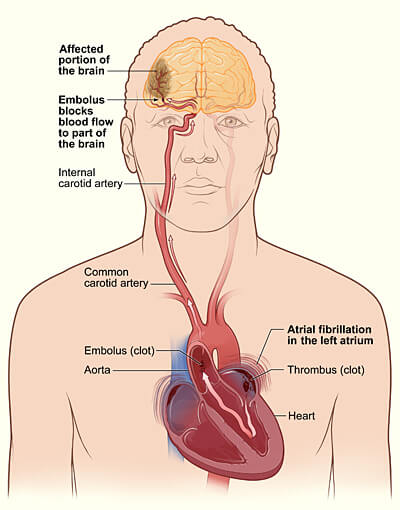
The figure shows how a stroke can occur during atrial fibrillation.
Heart failure
Heart failure occurs if the heart can not pump enough blood to meet the body's needs. MP can lead to heart failure, because the ventricles are reduced very quickly, which is why they are not completely filled with blood. Thus, they are not able to maintain blood circulation at the proper level.
Persistent MS with an uncontrolled fast heart rate of the ventricles can cause such complications as dilation cardiomyopathy and lead to electrical remodeling in the atria (atrial fibrillation) The therapy in the form of atrioventricular node modification or permanent implantation of the pacemaker, for controlling the contractility of the ventricles, can improve their function and quality of life indicators.
Forecast
Atrial fibrillation is associated with an increased risk of developing dangerous complications and mortality, partly due to the increased likelihood of developing thromboembolic lesions expressed by stroke.
A favorable prognosis is given in the case when the MP is able to restore sinus rhythm as soon as possible.
The development of atrial fibrillation contributes to the onset of heart failure, and when it is present, the severity of CH is deteriorating. Also, MF can complicate the course of heart failure in patients who depend on the atrial portion of cardiac out put.
When determining the patient's hypertension and heart valve damage, the risk of developing heart failure in the onset of MI increases. In addition, MS can cause cardiomyopathy-mediated tachycardia, especially if proper treatment is not performed.
Prevention
Following the correction of lifestyle and taking measures to reduce the risk of heart disease to prevent paroxysms of atrial fibrillation can help the following steps:
- You need to stick to dietary nutrition (DASH diet) with low saturated fats, trans fats and cholesterol. Healthy foods include a variety of whole grains, fruits and vegetables every day.
- You can not smoke.
- It is important to allow permissible physical activity.
- Worth supporting the weight within the normal range.
- If other heart disease or risk factors are detected, it is advisable to consult a physician to properly manage your condition.
- It is necessary to restrict or avoid drinking alcohol.
- It is important to monitor blood sugar, especially if diabetes is detected.
- It is necessary to undergo regular medical care and to take medication in accordance with the requirements.
Video Facts about the heart. Atrial fibrillation
