Constrictive pericarditis
Author Ольга Кияница
2019-03-03
Constrictive pericarditis (CP) is a relatively rare form of clinical heart failure. The true prevalence among the population is unknown, but among those who determine viral pericarditis, the disease, according to various estimates, occurs in less than 0.5% of cases. But since KP is a potentially reversible pathology, the diagnosis should not be missed.
The occurrence of constrictive pericarditis in rare cases is primary, most often its appearance is associated with other systemic diseases.
Laboratory tests with CP are not specific, therefore instrumental diagnostic methods are necessarily used. To prevent the development of serious complications, treatment is required, most often surgical. Most patients have a favorable prognosis.
Video: Constrictive pericarditis | causes, symptoms, diagnosis, treatment
Description of Constrictive Pericarditis
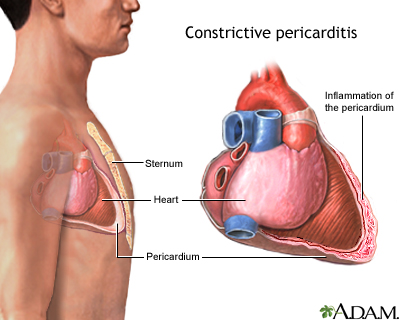
Constrictive pericarditis is a chronic inflammatory process, often characterized by chronic scarring, fibrosis and pericardial calcification. Its development is mainly associated with diastolic dysfunction of the heart, which ultimately leads to a decrease in cardiac output and heart failure.
Normal pericardium consists of two layers, that is, the inner serous layer and the outer fibrous layer. The pericardium has many functions to protect the heart and preserve normal heart function, including maintaining mechanical effects on the heart. The pericardium also has immunological, paracrine, vasomotor and, most importantly, fibrinolytic activity.
[1 - Shabetai R. Pericardium. Norwell (Massachusetts): Kluwer Academic Publishers; 2003. p.1-50].
Pathophysiology of constrictive pericarditis
In the normal state, the pericardium minimally impedes ventricular distensibility with normal heart workloads. With KP, a change in the structure of the pericardium creates a rigid ventricular-pericardial reaction. This leads to an increase in diastolic pressure and a more rapid increase in ventricular pressure for venous return.
Inflamed pericardium in combination with constriction restricts ventricular relaxation and increases ventricular diastolic pressure, which leads to an increase in diastolic pressure in all chambers. Clinically, it manifests itself mainly as right-sided hyperemia (stretching of the jugular vein, edema, and ascites).
An increase in pressure in the pulmonary capillary bed and a decrease in cardiac output in response to physical exertion (with insufficient filling of the ventricles) lead to shortness of breath and intolerance to physical activity. As a result, pulmonary edema develops, which is less common, or typical systolic heart failure.
When the CP is due to the fact that the heart is surrounded by inappropriate pericardium, the normal decrease in intrathoracic pressure during inspiration is not transmitted to the intracardiac pressure. This effect enhances the inspiratory decrease in pulmonary venous pressure (since the pulmonary veins are mainly located extrapericardially).This leads to a reduction in the left left inspiratory preload, further reducing the left side inspiratory volume. Multimodal diagnostic assessment of KP confirms these results, facilitating diagnosis.
Signs of Constrictive Pericarditis
Symptoms of pericarditis may include the following:
- Acute chest pain.
- Cardiopalmus.
- Shortness of breath, especially when bending.
- Minor fever.
- General weakness.
- Swelling of the abdomen or legs.
- Cough.
- Pain in the shoulder or back.
Chest pain with pericarditis can be characterized as follows:
- Sharp and piercing (caused by friction of the pericardial leaflets).
- The pain may worsen when the patient coughs, swallows, takes deep breaths, or lies flat.
- The feeling of relief comes when the patient is sitting or leaning forward.
- The patient may also feel the need to bend down or press down on the chest in order to breathe more comfortably.
Symptoms for pericarditis are often very similar to a heart attack. If you have any suspicions, you should definitely seek medical help, especially if you have chest pain or other signs above. The doctor will be able to exclude less serious diseases and find out the cause of pericarditis.

The cause of constrictive pericarditis
Idiopathic pericarditis remains the predominant cause of CP in the countries of the Western world, followed by surgery caused by radiotherapy.
Tuberculous pericarditis is still the main cause of KP in developing countries and in immunocompromised patients.
Complete pericardectomy, if possible, remains the only definitive cure for the disease. KP can be prevented in some patients; however, most often its development cannot be prevented.
Video: CONSTRICTIVE PERICARDITIS BY NIK NIKAM MD MHA
Diagnosis of constrictive pericarditis
To install the primary diagnosis of CP, a physical examination of the patient is required. Patients with a history of cardiac surgery, radiation or tuberculosis in history and in combination with edema, abdominal distension and shortness of breath during exercise require special attention. In this case, the doctor may note the following features of an objective examination:
- The presence of increased jugular venous pressure , which is determined in almost all patients not suffering from hypovolemia.
- A symptom of Kussmaul when a pericardial restriction results in the inability of the right heart to pump the required blood volume, which leads to an increase in inspiratory pressure in the jugular veins.
- High pericardial noise spreading along the left sternal border and determined by auscultation.
- Ascites and significant swelling of the lower extremities , formed as a result of blood accumulation and plasma leakage into the surrounding tissues due to heart failure.
Echocardiography
As an initial diagnostic test, echocardiography can confirm the diagnosis of CP in most cases, especially if the likelihood for a quality test is high enough. Echocardiography (echoCG) shows signs of both exaggerated ventricular interdependence and intrathoracic-intracardiac dissociation.
Characteristic for KP is the detection of the displacement of the septum . In addition to this feature, there is also an abnormal movement of the septum between the strokes, or the so-called “shiver”, which is caused by the differential rapid early diastolic filling of the right and then the left ventricle. Changes in the system of the inferior vena cava, hepatic veins and a decrease in diastolic direct flow may also be noted.

X-ray of the heart
In CPs, chest x-rays may exhibit pericardial calcification characteristic of clinical heart failure and increased pressure in the portal vein system.
Computed tomography and magnetic resonance imaging
Chest CT scan is more sensitive to pericardial calcification than chest radiography. CT scan of the chest and MRI can accurately measure the thickness of the pericardium, in particular, MRI demonstrates excellent accuracy (93%) in determining the thickening of the pericardium more than 4 mm. However, it is important to remember that up to 18% of cases of surgically confirmed CP may have a normal pericardial thickness, despite the pathological inconsistency.
Minor changes in the pericardium, which can be visualized using echocardiography, CT or MRI, also often indicate the presence of CP. MRI transmits information about active pericardial inflammation, which can help in making therapeutic decisions. In addition, an MRI scan of the heart provides a unique assessment of the myocardium, which can identify cardiomyopathic processes when the diagnosis is uncertain.
In contrast to echocardiography, CT and MRI of the heart do not depend on the patient’s habitat and can provide better cardiac imaging when echocardiographic imaging is not optimal. Respirophasic shifts in septum movement are well defined both in CT and MRI. In addition, CT and MRI can provide information about alternative causes of dyspnea, such as lung disease or diaphragmatic paralysis.

Additional heart diagnostics
Cardiac catheterization remains the gold standard in the diagnosis of CP, especially if non-invasive testing was inconclusive for assessing the presence of constriction and evaluating hemodynamic significance. Although most patients with CP do not require hemodynamic catheterization for diagnosis, one of the subgroups of particular concern is patients with radiation-induced heart disease. It is often difficult for them to determine the extent of restrictive cardiomyopathy, even if narrowing symptoms are present.
Even with high-quality echocardiography and radiology of the heart, these patients may require invasive hemodynamic catheterization to assess the increase in filling pressure with diastolic alignment, ventricular interdependence, and intrathoracic-intracardiac dissociation.
Laboratory studies with CP are not specific. A high level of BNP (sodium diuretic peptide) may suggest a greater likelihood of restrictive cardiomyopathy, but studies have shown a significant coincidence of diagnostic values in this population that limit clinical utility.
Constrictive pericarditis treatment
The main goal in the treatment of KP is to improve cardiac function. It is very important that the primary etiology is identified and managed accordingly.
The final cure for CP is primarily a surgical procedure in the form of complete pericardiectomy, where possible.
Pericardiectomy usually leads to rapid hemodynamic and symptomatic improvement in most patients. However, in some cases, especially in the presence of left ventricular systolic dysfunction, as well as concomitant diseases, symptoms may persist after surgery.
Drug treatment for the purpose of careful observation or symptomatic treatment is carried out in less serious cases. Yet this treatment option remains controversial.
Management of CP is different from the treatment of acute pericarditis, where it may be useful to use non-steroidal anti-inflammatory drugs (NSAIDs), cyclooxygenase inhibitors (COX) -2, colchicine, corticosteroids, or combination therapy .
The main features of this type of treatment:
- Diuretics are mainly used in the early stages of the disease to improve pulmonary and systemic hyperemia.However, drugs from this group should be used with caution, as any decrease in intravascular volume can lead to a significant drop in cardiac output. In some patients, severe fluid restriction and a low-sodium diet may be recommended. It is important to anticipate the complications that may arise due to the failure of early diagnosis of SR or improper treatment of narrowing, as well as complications associated with the primary etiology of narrowing or associated with any existing pathology.
- Subacute CP may react to steroids (hormones), especially if drugs from this group were used before the development of pericardial fibrosis.
- Any other medications used to treat patients with KP should be specifically directed to the etiology of pericarditis. In particular, for tuberculosis, anti-tuberculosis therapy is appropriate.
- KP-related complications may require the use of their own specific therapy, for example, antiarrhythmic drugs .
In general, beta-blockers and calcium channel blockers should be used with caution, since sinus tachycardia, which usually occurs during constriction, has a compensatory function. It is used to support cardiac output when adjusting a fixed stroke volume (secondary to a fixed diastolic filling).

Pericardiectomy: prognosis and precautions
Morbidity and mortality are most often associated with preoperative atrophy or myocardial fibrosis, which can be detected using modern methods of cardiac imaging, including computed tomography. These atrophy or myocardial fibrosis and decreased mobility of the ventricles, especially the free wall of the right ventricle.
In addition to myocardial atrophy or fibrosis, other important factors leading to long-term recovery from pericardiectomy include incomplete decortication as well as recurrent contraction, which can lead to prolonged cardiac compression associated with persistent mediastinal inflammation and fibrosis.
Additional prognosis can be affected by the presence of extensive pericardial calcification. Most importantly, these calcifications can spread to the myocardium, making pericardectomy bulky and complex, leading to perioperative bleeding, hemodynamic instability, and subsequent death.
Precautionary measures
In the postoperative period, low cardiac output can be observed in patients with severe symptoms caused by progressive disease or exhaustion. Also often seen in patients with ascites or other signs of fluid retention. In such cases, patients need rigorous perioperative measures and an experienced surgeon to avoid imminent death. In particular, it may be necessary to maintain high pressure in the left atrium, sympathomimetic injections or both to maintain cardiac output during this critical period.
Mechanical support of the circulatory system, such as extracorporeal membrane oxygenation, counterpulsation of an intra-aortic balloon, or an assistive device system, should be used in critical conditions. In addition, treatment should be carried out to prevent the development of acute pancreatic insufficiency in the form of supporting parameters, thus avoiding early mortality after pericardectomy.
Conclusion
In some cases, the primary causes of constrictive pericarditis can be identified and eliminated, which may be helpful in preventing recurrence or further narrowing. Sometimes KP is impossible to prevent.
Pericardiectomy remains the only definitive treatment for constrictive pericarditis. Pericardiectomy, especially in its full version, is shown after confirming the diagnosis of CP. Most importantly, pericardectomy is recommended at early stages during the period of constriction, while patients still have a favorable functional state. This allows you to achieve favorable results in the short and long term.
Medical therapy is most often directed to the primary etiology of constriction, if possible. When identifying the cause, all valid measures should be taken to eliminate it.
Video: Cardiac tamponade vs constrictive pericarditis
