Surgery for congenital heart disease
Author Ольга Кияница
2018-12-01
Congenital heart defects (CHD, cardiac abnormalities) are structural disorders of the heart and adjacent vessels that were formed at the stage of the intrauterine development of a child. At present, CHD is determined in 1% of all children with birth defects, which is considered to be a rather high indicator.
There are various types of congenital heart defects and the most common is ventricular septal defect (31% of cases).
For the diagnosis of CHD using modern methods of research on the type of ultrasound of the heart. Additionally, electrocardiography, MRI, angiography, endoscopic diagnostic methods are performed. Before the operation, the patient is prepared, the postoperative period is also important.
Video: Live Great! Heart disease
Key points
- Types of surgery for congenital heart disease and the results of its implementation mainly depend on the specific heart defect in a child (its severity, duration of existence and associated disorders).
- The physical parameters of the child (height and weight) must reach a certain point before the operation can be performed, although in extreme cases it is done without delay.
- Types of surgical procedures include palliative surgery, cardiac catheterization, balloon angioplasty, artery switching procedure, Bleloc-Taussig anastomosis (BT), and Norwood's surgery.
In addition to monitoring and drug therapy, the negative effects of the heart defect can be reduced or, possibly, almost eliminated by surgery. The types of surgery and the typical outcomes of surgical interventions primarily depend on the specific heart disease.
The height and weight of the child must reach certain indicators before surgical interventions can be performed. Heart surgery requires a certain amount of strength to recover. In addition, extracorporeal membrane oxygenation (ECMO) may be necessary during and, possibly, after surgery.
ECMO is a medical device that is located outside the body in order to replenish the functions of the heart and lungs.
It should be noted that any operation is associated with risks. The presence and severity of postoperative complications depend on the type and complexity of the surgical intervention, as well as on the type and severity of congenital heart disease.
Types of surgery
Palliative intervention
Palliative surgery refers to procedures in which the complete recovery of a heart defect is not possible, and the blood flow is controlled either by anastomosis or by an artificial tube implanted in the heart or in one of the ventricles of the heart.
After performing a palliative surgery, the heart often decreases its functionality, which leads to an insufficient amount of oxygen being delivered.
Babies after palliative surgery can live for a long time, although as they grow, their lifestyle cannot be as active as in children and adults with a normal heart. Other children with this condition and without treatment may not survive at all or live a short life.
Heart catheterization
The operation called cardiac catheterization, or minimally invasive surgery, is based on the use of a thin flexible tube (catheter).
The goals of cardiac catheterization may be different, in some cases they are carried out during the same procedure:
- To gather information, then talk about diagnostic catheterization.
- To perform surgery, also called interventional catheterization.
Through a tiny incision in the arm, neck, or groin, a catheter is inserted into a blood vessel (artery or vein) and guided to the heart under the control of a real-time x-ray or fluoroscopy.
If necessary, catheters can be used to take blood samples, measure pressure, inject dye (for angiography) or restore the structure of certain areas of the heart and surrounding blood vessels.
Heart catheterization is performed at any age, from babies to elderly patients. Sedation varies from local anesthesia to general anesthesia, it all depends on the type of procedure. A minimally invasive operation is performed in the cardiac catheterization unit, which looks like a small operating room.
Video: Pediatric heart surgery: heart surgery, congenital heart defects in children
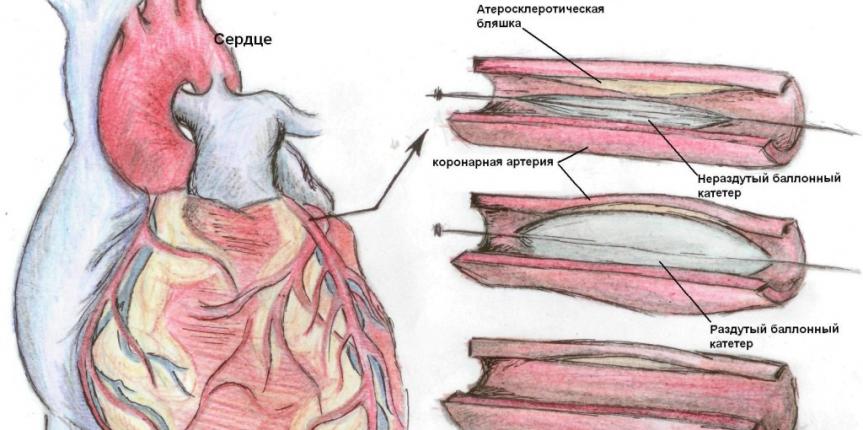
Heart balloon angioplasty
When any part of the circulatory system of the heart becomes constricted, balloon angioplasty, also known as balloon dilation, can help open the constricted area and improve blood flow.
The main task is to direct the catheter with a balloon at the tip to the heart, where air is forced into it to open the constricted area or to expand the stenotic opening.
Principle of surgery
- Thin tubes, called catheters, are inserted into the blood vessels in the groin in the upper leg. Usually, x-rays are taken in parallel and the constricted area is measured.
- A balloon catheter (only in a deflated state) at its tip passes through the first catheter to this constricted area.
- As soon as the cylinder is delivered to the required place, it is opened, forcing air, which contributes to the opening of the constricted area.
- The balloon causes the narrowed area to expand, and if necessary, stretches the walls of the vessel.
- The balloon is blown away, the catheters are removed, and the entry point on the leg is closed with a bandage.
It is important to know that after balloon angioplasty, the affected area may narrow again or even close, blocking the blood flow. To prevent such complications after expansion, a stent is inserted, which is a wire mesh. Its use allows you to keep an open area in full condition.
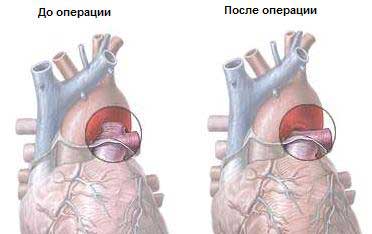
Arterial switching operation
Arterial switching is shown to those babies who have defects according to the type of transposition of the great vessels (TMS). With this defect, the position of the main vessels (the aorta and the pulmonary artery) is disturbed, as a result of which the blood is incorrectly directed from the heart to the lungs and the body. With this pathology, the blood, which has already been enriched with oxygen in the lungs, goes back here, while the blood, which needs oxygen, continues to circulate throughout the body.
There are several options for transposition, and if the body is completely oxygen-deficient, then this CHD is very serious and may even lead to a fatal end.
Arterial switching surgery, usually performed during the first few weeks of life, is essential for correcting hemodynamics.This open-heart procedure consists of the “switching” of the pulmonary artery and aorta, that is, they are placed in normal positions and the coronary arteries are attached to the new aorta in the places intended for it.
It is important to note that before the operation is performed, the patient is injected with a drug called prostaglandin, which maintains the arterial duct in the open state in order to improve blood circulation.
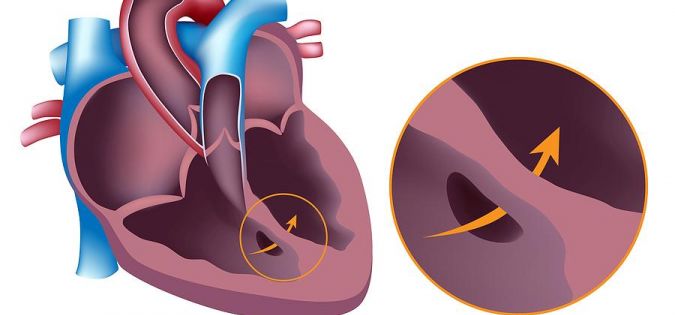
Another temporary procedure that can help with blood mixing is balloon atrial septostomy, in which a hole is made between the left and right atria. This type of surgery for congenital heart disease is used to temporarily support the child until he is old enough to withstand surgery to restore normal blood circulation.
After surgery, in the long run, large vessels may narrow, which will require balloon angioplasty or another suitable surgical procedure. In addition, the coronary artery, which must be re-implanted in a new location, can be deformed, leading to a decrease in blood flow to the heart. Additionally, protection against bacterial endocarditis, which as a complication may occur after surgery, must be made.
Blast-Taussig Anastomosis
This type of surgery is used to correct defects that affect the flow of blood from the right ventricle, through the pulmonary artery, and further into the lungs. These include atresia of the pulmonary trunk, stenosis of the pulmonary trunk, atresia of the tricuspid valve, and stenosis of the tricuspid valve.
BT anastomosis is often performed with “blue” congenital defects and is considered a palliative procedure, since it does not completely correct the defect. It helps to reduce the severity of symptoms until the child is older, to be ready for another type of operation.
Anastomosis is a small tube made of a synthetic material called Gore-Tex. With its help connects the area of the aorta and the pulmonary artery, resulting in a kind of workaround. This allows mixed blood, from oxygenated and deoxygenated, to pass through the lungs again and be saturated with plenty of oxygen.
The anastomosis plays the role of the ductus arteriosus and is often put into action after the natural AP is closed. With its help, heart function is improved, with more blood passing through the lungs and saturated with oxygen. As a result, cyanosis or blueness of the skin, which is often determined in children with blue defects, is eliminated.

Blast-Taussig anastomosis: a) original procedure; b) a modified procedure.
Anastomoses are usually used for four to five months until the baby outgrows them. In the future, you will need a second operation or a final reconstructive reconstruction.
Operation Norwood
This type of surgery is used in cases where only one pumping chamber of the heart (one ventricle) is detected. Also used for other isolated ventricular defects.
Norwood's surgery may be part of a series of surgical treatments. In particular, the aorta can be reconstructed using the pulmonary artery so that the ventricle can easily pump blood throughout the body. A BT anastomosis is also to be placed to maintain blood flow through the lungs and a bi-directional Glen anastomosis. At the last stage, the Fontaine palliative surgery is performed.
The risks associated with the operation of Norwood are quite high. This is a large and complex surgical procedure that requires expert assistance before, during and after surgery. The interaction between the cardiologist, the cardiac surgeon, the anesthesiologist and all other support staff is very intense. Mortality can reach 20% even in the best centers. The potential for complications is also high.

After the first stage of Norwood's operation, the heart is very weak, so the enrichment of oxygen in the lungs completely depends on the anastomosis of BT. The risks associated with BT shunt are most often expressed in a high probability of developing blood clots in artificial devices. In the postoperative period, patients must take anticoagulants, such as heparin.
Once the child has recovered from the first operation, two other surgical interventions can also be performed: the Glenn operation, or the second stage, and the Fontana operation, or the third stage. The long-term results of this third procedure are not known, since the “oldest” patients who survived this surgical operation today are at the age of 20 years.
Finally
All congenital heart defects, even insignificant at first glance, require careful monitoring by a cardiologist, and sometimes a cardiac surgeon. Both the surgical operation itself and the postoperative period are extremely important in the effectiveness of the treatment of the patient.
Video: Facts about the heart. Congenital defects of the septum of the heart
Similar articles
During fetal development of the fetus under the influence of predisposing factors, normal formation of the cardiovascular system may be disturbed. As a result of this, congenital malformations are created that can be compatible and incompatible with life. The development of pathology is often associated with the wrong way of life of the mother during pregnancy, although in some cases, heredity plays a big role.

There are cardiovascular diseases that can lead to permanent loss of disability. In order to prevent such complications, timely treatment should be performed. Therefore, in identifying the acquired heart defects, it is not necessary to delay with the implementation of medical recommendations.

One in 120 babies is born with a heart malformation. Some of them are heavy, but in most cases, they do not represent danger. Defects may include abnormal walls or heart valve shapes, as well as blood vessels that fit or depart from the heart.
