Hemorrhagic stroke
Author Ольга Кияница
2018-06-27
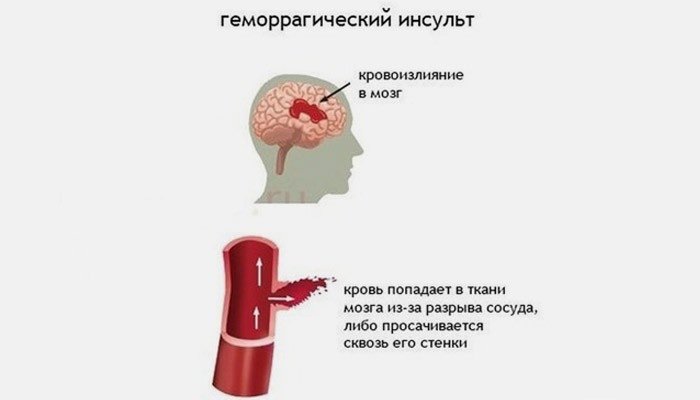
Hemorrhagic stroke (GI) refers to spontaneous (non-traumatic) intracranial hemorrhage, which can occur in several types, including intracerebral or parenchymal hemorrhage (PKI), intraventricular hemorrhage (IVF), and subarachnoid hemorrhage (SAKI).
Intracerebral haemorrhage is most widespread and mainly develops at the age of 45 to 60 years.
Often, before the development of GI, a person is longly ill with hypertension, a blood disease, cerebral atherosclerosis. If in addition to this the patient often experiences emotional or physical overstrain, then the clinic develops against a background of tension.
Video: Hemorrhagic stroke
What is a hemorrhagic stroke?
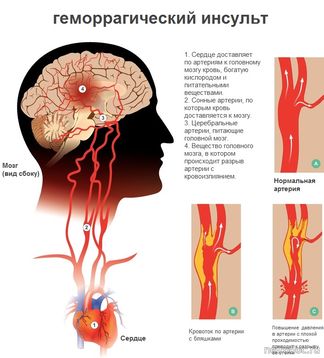
Hemorrhagic strokes occur when a blood vessel that supplies blood to the brain is torn and blood comes out of it into the brain tissue. In this case, brain cells and tissues located below the rupture site may not receive oxygen and nutrients. In addition, bleeding exerts pressure on surrounding tissues, causes inflammation and swelling. The development of hemorrhagic stroke can lead to serious damage to the brain.
Hemorrhagic strokes are divided into two main categories:
- Intracerebral hemorrhage (intracranial hemorrhagic stroke, ICGI) . Bleeding occurs from the blood vessels of the brain.
- Subarachnoid hemorrhage (subarachnoid hemorrhagic stroke, SAGI). Bleeding is in the subarachnoid space, which is located between the brain and the membrane covering the brain.
Statistics on hemorrhagic stroke
- The estimated incidence of primary intracranial GI is 1-2 / 100,000 per year in North America.
- ICGI accounts for about half of all cases of stroke among children.
- On newborns it is necessary about 20% -30% of all cases.
- Boys are more prone to GI than girls, 60% compared to 40%.
- The main causes of GI include atrioventricular malformations of 40%, coagulopathy 20%, cavernous 10%, aneurysm 10%, others 20%.
Causes of hemorrhagic stroke
Causes of hemorrhage in the brain:
- Head injury. Trauma is one of the most common causes of bleeding in the brain in young children.
- High blood pressure . Hypertension is more common in adults, but high blood pressure can occur in infants, children and adolescents. Arterial pressure should be extremely high to cause the development of hemorrhagic stroke. Most often, this can cause a hemorrhagic stroke, when there is high blood pressure inside a weak or abnormal blood vessel.
- Aneurysm . Pathology is the weakening of the wall of the blood vessel, which swells and protrushes. A weakened blood vessel may burst or through it a blood plasma seeps into the surrounding brain tissue, thereby causing a hemorrhagic stroke.
- Propensity to bleeding . Hemophilia and sickle-cell anemia can cause abnormal bleeding, as the process of blood coagulation is disrupted. Other conditions, also known as thrombocytopenia, are characterized by a decrease in platelet count.
Platelets help to coagulate blood and help prevent its loss in damage to blood vessels. A lower level of platelets can cause a massive hemorrhage into the surrounding tissues, since the body is weakly able to form a thrombotic clot that covers the site of damage in the vessel.
- Diseases of the liver . Various inflammatory and infectious diseases of the liver are associated with increased bleeding due to a lower level of clotting factors.
- Tumors of the brain . When a brain tumor begins to bleed, it can cause symptoms similar to those of a hemorrhagic stroke.
Also, the cause can be neonatal vitamin K deficiency, arteriovenous malformations (AVM).
Genetic syndromes or known mutations contribute to a minority of cases, including the following:
- Coagulopathies (hemophilia)
- Autosomal dominant cerebral cavernous malformation
- Hereditary hemorrhagic telangiectasia (NGT)
- Syndrome of Alagil
- Microcephalic primary dwarfism with cerebral arteriopathy / aneurysms
- Hereditary angiopathy with nephropathy, aneurysm and muscle cramps
Symptoms of hemorrhagic stroke
In hemorrhagic stroke, there may be different symptoms. Their nature often depends on the type, location of the affected brain and the main cause of the stroke. If extensive areas of the brain are affected, the symptoms can be more serious.
The common initial manifestation of hemorrhagic stroke, especially in children, is convulsions . During convulsions, babies can turn their backs and bend their limbs or experience spasms throughout the body. Infants and children may tremble or feel cramping on one or both sides of the body.
Other symptoms of hemorrhagic stroke include extremely severe lethargy and drowsiness , as well as hemiparesis(one-sided weakness). Older children may experience speech problems or complain of a severe headache.
Additional common symptoms include:
- vomiting;
- convulsions;
- meningeal symptoms;
- fever.
Sometimes the symptoms of hemorrhagic stroke appear suddenly, but sometimes a hemorrhagic stroke occurs slowly and with a steady deterioration of the patient's condition.
Diagnosis of hemorrhagic stroke
If any symptoms of GI appear, you should immediately call an ambulance or go with the patient with any transport to the nearest hospital.
Diagnosis of hemorrhagic stroke begins with the study of medical history and physical examination. Medical workers may ask about injuries or head injuries, infection, developmental delay, and the existence of a family predisposition to bleeding.
With an objective examination of the patient, signs of weakness and numbness of the limbs, as well as other symptoms of stroke, can be detected.
Laboratory diagnosis of hemorrhagic strokes may include:
- A general blood test with counting the number of platelets.
- Coagulation profile, including prothrombin time / partial thromboplastin time.
- Comprehensive metabolic profile, when it comes to liver or kidney disease.
- Screening of the rheumatologic panel for suspected inflammatory diseases.
- Bacteriological analysis of blood if suspected mycotic aneurysm or other acute inflammatory diseases.
- Genetic diagnostic studies if there are specific genetically determined vascular syndromes (eg, family cavernoma, Alagil syndrome).
Visualization studies allow us to see the localization of the violation and its dimensions in absentia. For this, the following diagnostic methods are most often used:
- Computed tomography (CT) of the head : the method is widely available and provides a sensitive and specific diagnostic confirmation of the presence of hemorrhage. This is an important first step in the surgical identification of hydrocephalus, which is a common acute complication of GI. Often, patients have a desire to avoid radiation exposure, so for such cases, CT is not appropriate. Yet this is the best and fastest way to determine possible neurosurgical emergencies.
- Magnetic resonance imaging (MRI) of the brain : after the initial diagnosis of GI and CT of the head, MRI is usually the next best study that allows you to accurately and accurately characterize the cause of hemorrhage, as well as the degree and nature of the parenchymal trauma. For example, the cerebral cavernoma is best diagnosed with MRI and is not diagnosed by other vascular imaging techniques. Also, the method allows the best identification of small foci of hemorrhage, cardioembolic pathology and cerebral venous thrombosis, as a frequent cause of hemorrhage.

- Vascular Imaging : This method is non-invasive and can be combined with MRI in the form of MRI angiography (MRI) or CT scan in the form of CT angiography (CTA). Used as a previous study for catheter angiography and in the planning of surgical intervention for strokes. The above methods are not sensitive to small aneurysms (
- Catheter angiography : this method of visualization is necessary for the planning of surgical treatment and for the final diagnosis of neoplasms and aneurysms.
- Cranial ultrasonography : it is often used to diagnose newborns when screening with the advantages of the bedside technique is necessary.
- Transcranial Doppler : sometimes used as a baseline study in the presence of signs of vasospasm in the case of an aneurysmal lesion. This method is not widely used in pediatric hospitals, since it is technically difficult to perform when diagnosing pathologies in young children.
Treatment of hemorrhagic stroke
The type of treatment will depend on the cause and severity of the stroke, as well as on the patient's age.
Treatment of hemorrhagic stroke most often includes:
- Infusion of liquids to prevent reverse dehydration
- Anticonvulsants for the prevention and control of seizures
- Blood transfusion
- Surgical effects to control bleeding or relieve pressure on the brain
Treatment of GI in acute period
The main methods of therapy are directed to the respiratory tract, the circulatory system. In patients with a depressed mental state, which rapidly worsens the general condition, the normal passage of the airway is ensured and ventilation is monitored. Also, adequate vascular access is provided and perfusion / oxygenation by liquids and vasopressors is maintained as needed.
Metabolic fluids allow the preservation of normoglycemia and normovolemia, which ensure a normal acid-base balance and an electrolyte state.
The hematological status of coagulation is restored with the help of blood preparations or fresh frozen plasma, and transfusion can also be performed to normalize the hematocrit.
Anticonvulsant therapy - helps prevent the risk of worsening of intracranial hypertension or rebleeding. Continuous monitoring of electroencephalography (EEG) may be required at the bedside of the patient or if the patient is treated with neuromuscular blockade.
Treatment of an acute condition aimed at normalizing the work of the brain
With intracranial hypertension, one or more strategies may be required, including:
- external ventricular drainage;
- evacuation of the hematoma;
- hemicraniectomy;
- hyperosmolar therapy (3% physiological saline solution).
With subarachnoid GI, vasospasm control (thorough clinical studies, possibly transcranial Doppler monitoring) and prevention by the calcium channel blocker (nimodipine) for 14-21 days are necessary.
Surgical and / or endovascular treatment of vascular anomalies - resection of an aneurysm, resection or embolization of arteriovenous malformation or resection of a cavernoma.
Most of the arteriovenous malformations of the Galena veins are eliminated by embolization.
Inoperable lesions can be subjected to radiation therapy - a gamma knife or proton beam.
After acute treatment, rehabilitation therapy begins in the intensive care unit as soon as possible. Improvement of the general condition allows for rehabilitation in the hospital.
Video: Recovery after Hemorrhagic Stroke
Long-term treatment
Arteriovenous malformations can be re-formed / restored, which is associated with a significant risk of re-hemorrhage.Subsequent angiography by the catheter is usually performed at regular intervals, approximately 18 years later. MRI angiography and CT angiography are unable to detect small AVM.
Anticonvulsants can be treated in several ways. One of the options - therapy with appropriate drugs for 3-6 months, which allows you to complete the initial surgery and rehabilitation. Factors affecting the course of the disease include the presence of residual or untreated AVM or aneurysm, the side effects of the drug and the presence of significant epileptiform changes in the EEG.
Strong psychosocial support is needed for the patient and family, ideally associated with long-term community-based rehabilitation services and individually developed programs.
Possible side effects associated with each treatment option:
Options for the final treatment of major vascular anomalies that cause intracranial GI have certain risks and benefits.
- Surgical resection of AVM or aneurysm can be successful and rescue, restoring blood circulation in the brain, but at the same time there is a risk of damage to normal vessels and adjacent brain tissues. The estimated risk of re-hemorrhage from untreated AVM or aneurysm is 4% per year. Some AVM are located in areas inaccessible to surgery, which causes serious neurological injuries.
- Embolization of AVM or aneurysm has the advantage that it is less invasive and therefore has fewer risks of damaging normal vessels and brain tissue compared to surgery. But at the same time there is still a possibility of disrupting the structure of a full-fledged vascular network, and hemorrhagic complications can also occur.
- The advantage of radiotherapy in the treatment of AVM lies in the fact that compared to surgical intervention, the area of damage to adjacent brain tissues is reduced. Such methods can be successful, although a smaller part of the total cure of the lesion is determined, so it is often necessary 12-18 months to achieve the intended effect of therapy.
Additionally, many patients do not tolerate the effects of radiation toxicity.
Forecast of hemorrhagic stroke
Prognostic findings on intracranial GI vary widely. Group studies report the results as follows:
- Mortality: mortality ratio from 7% -50%, that is, an average of about 25%, in studies for the 1970s - 2004. In the most recent group studies with aggressive surgical intervention, mortality lies within the lower part of this range.
- Neurological status of survivors: with a "good" result, about 30% -50% of patients reported surviving.
- Long-term diseases that occur after GI include chronic headache and epilepsy, although the indicators of these problems are not well characterized.
Factors associated with a high risk of poor outcome include a large amount of hemorrhage (> 2% of the total brain volume) and depressive mental status during examination.
Prevention of hemorrhagic stroke
There are no proven or generally accepted methods of screening and preventive treatment of GI, except for the elimination of conditions that predispose to its development. Most cases of AVM and aneurysms are isolated and non-syndromic, so they are asymptomatic until they show up as a hemorrhage.
With known genetic syndromes associated with aneurysms, AVM, etc., there is no definite proven strategy for visualizing surveillance or performing pre-symptomatic surgical or endovascular therapy. Such decisions are made in each specific case under the guidance of individual practitioners.
Video: Hemorrhagic stroke. Hemorrhage in the brain

Какой только дряни нет… Инсульт вообще, вещь страшная, конечно. Я целиком и полностью полагаюсь на профилактику. Думаю, что она меня спасет. Принимаю гинкоум, стараюсь больше спать, не есть жирного много… Сосуды по узи стали более эластичными и не забитыми, кровь пожиже стала. Так что не все так страшно, если заботишься о себе))