Bacterial endocarditis: causes, symptoms and treatment
Author Ольга Кияница
2018-09-28
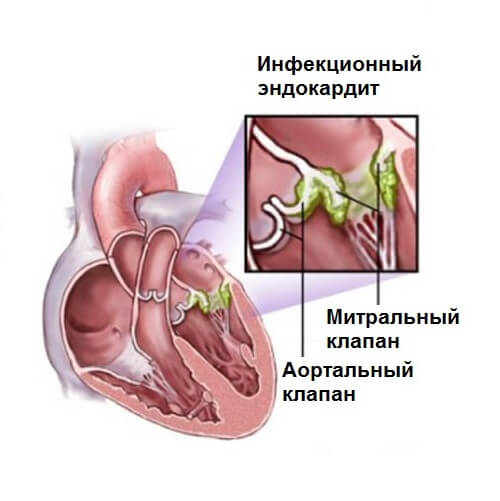
Bacterial endocarditis (EB) is an inflammation of the endothelium of the heart (inner cardiac membrane), which often goes to the heart valves. In severe disease, a complication such as heart disease can often occur, which in turn can lead to heart failure.
Endocarditis with novolat. endocarditis from ancient Greek δνδον “inside” + καρδία “heart” + itis “inflammation”. Literally means inflammation of the inner lining of the heart - the endocardium.
According to the Encyclopedic Dictionary of Brockhaus and Efron: in 86 tons (82 tons and 4 extra). - SPb., 1890-1907.
For the examination of patients with suspected BE, various diagnostic methods are used. First of all, an ultrasound of the heart is done, and this study, if necessary, is supplemented with bacterial blood tests, electrocardiography, phonocardiography.
Video: Bacterial endocarditis
Bacterial endocarditis statistics
- The annual incidence is 5-7 cases per 100,000 (Fraimow 2013).
- In the United States, between 40,000 and 50,000 new cases are registered annually, with the average payment for a hospital exceeding $ 120,000 per patient (Bor 2013).
- It develops more frequently in men than in women (approximately 1.5: 1 - 2: 1) (Moreillon 2010).
- Nosocomial mortality is 14–22%, with a 1-year mortality rate of 20–40% (Gomes 2017).
- Prior to the widespread use of antibiotics and surgical treatment, bacterial endocarditis was almost a common fatal disease (Aretz 2010, Osman 2013).
Description
Bacterial endocarditis can manifest itself in various forms, which depends a lot on the nature of the disease:
- Acute form - lasts several weeks.
- Subacute form - proceeds for 2-3 months.
- Chronic form - it can develop for several years and at the same time is quite difficult to treat.
Depending on the associated disease are distinguished:
- Primary BE - is determined by direct lesion of the heart valves.
- Secondary BE - develops on previously affected heart valves or as a result of the development of rheumatic heart disease.
Pathophysiology
In the normal state and in the absence of damage, the endothelium of the valves is very resistant to colonization and infection by bacteria circulating with the blood.
Various microtraumas caused by turbulent flow, intracardiac disorders, etc., or chronic diseases (rheumatic heart disease, congenital heart defects, use of prosthetic valves, previously experienced EB) can damage the endothelium.
Damage to the endothelial sheath causes the formation of a thrombus from fibrin and platelets on it. Microbes can colonize this clot during transitional episodes of bacteremia, fungal infection, and viremia.

The most common risk factors are:
- Heart Disease / Damage (Most Risk).
- Use of narcotic substances.
- Low immune protection.
- Poor oral hygiene.
- Nosocomial infection.
Causes
Most often, the development of bacterial endocarditis is promoted by microorganisms, which with the blood flow accumulate on the valves of the valves and infect them. The following bacteria are of primary clinical importance:
- S. aureus (Staphylococcus aureus). The most common microorganism that causes EB. Patients usually get sick more clearly and faster. It is reported that the mortality rate with the participation of this bacterium reaches 47% (Moreillon 2010, Fraimow, 2013). May affect normal and abnormal valves.
- S. viridans (streptococcus). Contributes only to valve damage. Mitral and aortic valves are most often affected in cases of EB, ranging from 90% to 95% of cases.
- S. epidermidis (epidermal staphylococcus). Associated with malformations, usually within 1 month after the onset of the disease.
- S. bovis (streptococcus) - more common among the elderly.
- S. pnuemoniae (pneumococcal infection). Acute fulminant disease. Often affects the structure of the aortic valve. High risk of perivascular abscess and pericarditis.
- P. aeruginosa (Pseudomuscular bacillus).
- HACEK - Hemophilus spp., Actino-bacillus spp., Cardiobacterium hominis, Eikenella corrodens and Kingella kingii.Slow-growing gram-negative bacilli, which may require several weeks before they are found in culture. It is 1-3% of all cases of EB, with an average delay in diagnosis of 1-3 months.
Video: Endocarditis (infective, libman-sacks) - causes, symptoms, treatment & pathology
Symptoms
Bacterial endocarditis most often develops atypically (without fever and other systemic disorders): This is mainly true for the elderly with a weakened immune system and people with right endocarditis of the heart.
- Systemic manifestations
May develop as bacteremia or sepsis for an unknown reason. Also, EB is often associated with fulminant sepsis and cardiogenic shock. Such conditions are considered critical and require immediate medical attention.
- Heart manifestations
During an objective examination, cardiac noises first of all attract attention. For example, in 50% of cases new noises, sounds of blood regurgitation are determined. At the early stage of the disease, noise is usually absent.
In some patients, atrioventricular abnormal conductivity of the heart impulses is determined. They can be supplemented by an extended PR interval and heart block.
Heart failure (HF) is a complication of BE, but often the symptoms of the type of edema and shortness of breath are first determined during the development of the disease. In particular, HF can occur due to valvular stenosis, valvular failure, rupture of an infected valve, and abnormal operation of the conduction system.
- Valve failure
It is considered the most common complication of EB. It develops due to the destruction of the valve as a result of rupture or penetration. Also, the cause of the pathological condition may be the loss of support from the chord components or the valve ring.
- Embolic manifestations
Often this is the immediate cause of the development of EB. Such embolic complications can occur at any time throughout the course of the BE.
The overall prevalence of embolic manifestations ranges from 20% to 50%. After the start of antibiotic treatment, such risks are reduced, but pathology may occur.
Factors that increase the risk of thromboembolic events:
- Determination of pathological microorganisms by the type of S. aureus, Candida and Abiotrophia.
- The presence of vegetations of more than 10 mm.
- Mitral valve impairment.
- Renal emboli
In the presence of a renal embolus, an abscess, ischemia and a heart attack may occur, side pains, pyuria or hematuria appear. This condition is often confused with simple pyelonephritis, urinary tract infection or ureterolithiasis.
- Pulmonary embolism
Pulmonary valve infection occurs in <5% of patients. In this case, pulmonary embolism occurs exclusively in right-sided BE, especially if there is no parallel left-sided endocarditis or paradoxical embolism.
Both septic emboli and “soft fibrin platelets” can be detected, which often lead to pulmonary infarction and septic pulmonary abscesses. Additionally, pneumonia can be diagnosed.
- Cerebral embolism
It is noted in about 20% of patients with BE, with a mortality rate of 40%. Neurological manifestations occur in 40-50% of cases and are the second leading cause of death in patients with BE. The development of cerebral embolism causes complications such as stroke, arteritis, abscesses, aneurysms, encephalomalacia, and meningitis.
- Eye embolism
There may be painless conjunctiva or subconjunctival hemorrhage.

The formation of microemboli in the ocular vascular system can lead to visual impairment (including monocular blindness). An ophthalmologic examination may reveal retinal hemorrhages and Roth blemishes. These formations are not pathognomonic for EB, but their presence should be suspicious of the development of this disease.
- Splenic emboli
May cause flank pain or irritation of the diaphragm. In some cases, can occur as symptomatic changes.
- Peripheral (skin) embolism
It occurs in 5-15% of patients with BE. At the same time such complaints, painless hemorrhagic formations on the legs and arms can be determined. Their occurrence. caused by septic microembolism of skin vessels with the formation of small abscesses in the dermis.
The Osler nodes are determined, which are sensitive erythema nodosum in the area of the pads of the fingers and toes, towering above the skin. Side surfaces of the fingers and lower arms may also be affected.
Most of the literature reports that these lesions are associated with the precipitation of immune complexes by precipitation (Aretz 2010) or allergic vasculitis (Moreillon 2010), but later literature suggests that microembolism and the formation of microabscesses may also be the etiological factor (Gomes 2016).
Local pain usually precedes the appearance of a rash for several hours. Nodes can be determined from several hours to several days and after their permission they do not leave any consequences.

- Point hemorrhages
Linear lesions, ranging from reddish brown to black color, can be 1-3 mm long and mostly appear under the nail plate.Such lesions can also occur in scleroderma, trichinosis, SLE, rheumatoid arthritis, psoriasis, antiphospholipid syndrome, hematological malignant disease, renal failure and trauma.
Diagnostics
For the examination of a patient with suspected bacterial endocarditis, various diagnostic methods are used: laboratory tests, electrocardiography,
- Laboratory research
The definition of white blood cells (CCV) is not a strictly sensitive and specific analysis for BE. Their number may be normal, increased or decreased. Increased BPC is present in about 50% of patients with EB.
Urinalysis (AM) - approximately 50% of patients may have hematuria (due to renal embolism).
C-reactive protein (CRP) is a sensitive, but not specific, assay. This figure rises in 90-100% of cases. Immune complexes (or rheumatoid factor) are present in 50% of patients after 6 weeks of infection.
Definition of blood culture - you need to get 3 sets of cultures. Fences do before antibiotic therapy with an interval of 1 hour. In some cases, the volume of blood obtained is more important. If the patient is in an unstable state or acutely ill, blood sets can be obtained within 5–20 minutes, and then antibiotics are given as quickly as possible.
Serology - tests such as ELISA, complement fixation and indirect immunofluorescent tests for Chlamydia, agglutination test for Brucella melitensis, indirect fluorescence for Legionella pneumoniae, ELISA for mycoplasmal pneumonia are usually performed.
PCR (polymerase chain reaction) of specific microorganisms (such as Coxiella, Brucella, Bartonella, Legionella, Chlamydia).
Microbiology. About 80% of BE cases are caused by gram-positive organisms.
- Instrumental diagnostic methods
Electrocardiography . It does not help in the diagnosis, but can detect complications. The most common ECG results are: unremarkable sinus tachycardia. The following complications can be determined: acute myocardial infarction (secondary to the involvement of the coronary artery), conduction abnormalities (complete heart block, atrioventricular block and His bundle branches).
X-ray . There is no specific benefit for the detection of EB. Sometimes the definition of bilateral pulmonary infiltrates may indicate the presence of septic emboli.
Computed tomography . Well suited for the study of complications in the chest, abdominal cavity and small pelvis (abscesses, pseudoaneurysms, distal infarctions, septic emboli). Abscesses can be detected, leading to fistulas between the left and right sides of the heart.
Transthoracic echo . Considered the gold standard when performing the following tasks:
- Useful for finding heart complications (such as ventricular size / function, hemodynamic severity of valve lesions, etc.).
- Detects about 70% of vegetations larger than 6 mm; 25% of vegetations less than 5 mm.
- Up to 30% of patients after using TT echoes are counted as “possible” patients with BE due to ambiguous or negative results of echocardiography or blood cultures.
Transesophageal echo. Surpasses the TT echo, especially in identifying complications such as perforations, abscesses and fistulas.
Treatment
The process of air exchange, respiration and blood circulation is controlled first of all. Further, in accordance with the indications prescribed drugs: antibiotics, aminoglycosides, anticoagulants.
- Antibiotic therapy
Standard treatments include: vancomycin and ceftriaxone. If necessary, add aminoglycoside (eg, gentamicin), especially in the presence of enterococcal infections. Nevertheless, some researchers do not recommend the use of aminoglycosides and gentamicin in particular, since they may do more harm than clear benefits (Fowler 2006, Fernandez 2013, Galvalda 2007).
The duration of antibiotic therapy in normal cases is 4-6 weeks. Treatment with antibiotics is mandatory because it allows the destruction of inactive bacteria, grouped in the foci of infection. Some researchers suggest that with uncomplicated BE with normal renal function, an antibiotic can be treated for only 2 weeks (Cahill 2017).
- Anticoagulant Therapy
Anticoagulants are not always indicated for patients with bacterial endocarditis. They do not interfere with the formation or embolization of vegetative growths. The only patients already on anticoagulation with endocarditis should consider the following points:
- Anticoagulation is considered relatively contraindicated in active endocarditis due to the risk of hemorrhagic lesions in the CNS.
- If patients took anticoagulants before the development of endocarditis (for example, patients with a prosthetic valve), they should most likely switch to something like heparin. If hemorrhage or bleeding occurs, the anticoagulant should be discontinued.
With prolonged treatment with anticoagulants, you should regularly check blood for clotting.
- Surgical intervention
In some cases, a better outcome is observed after the operation than with constant medical treatment. Especially often perform surgical intervention in the left-sided endocarditis and. aureus endocarditis.
The main indications for surgery:
- Drug-resistant BE.
- Cardiogenic shock due to valvular failure.
- Persistent infection despite antimicrobial therapy.
- Fungal or other difficult-to-treat organisms.
- Determination of one or more emboli during the first weeks of antibiotic therapy.
- Complications of the type of dissection, perforation, fistula and large perivascular abscesses.
Other potential indications for surgery in patients with EB include:
- Refusal of antibiotic therapy.
- Vegetative growths of more than 10 mm, noted during echocardiography.
- Fungal endocarditis.
- Early endocarditis after arthroplasty (in the first 2 months after surgery).
- Re-embolization despite medical therapy.
Generalized endocarditis is usually not amenable to surgical treatment. Partly due to the high frequency of EB recurrence after the intervention.
Key points
- Endocarditis is a disease with a high degree of progression and mortality.
- Symptoms and signs of the disease can be very non-specific.
- It is possible to suspect pathology in any person with the appearance of new cardiac noises, bacteremia without clear localization, peripheral embolic manifestations.
- The diagnosis is usually based on instrumental examinations such as echocardiography, computed tomography, and laboratory tests.
- Treatment consists of antibiotics covering the most common pathogens. In the extreme case, the operation is performed, especially if the patient has valve failure.
Video: Treatment of infective endocarditis
Similar articles
Some heart diseases are more often manifested in the background of other pathological conditions. This category includes endocarditis, which in its development affects the heart valves to a lesser or greater degree. Since the valve apparatus plays an important role in the circulatory system, it is extremely important to undergo treatment in time when it is damaged.

There are cardiovascular diseases that can lead to permanent loss of disability. In order to prevent such complications, timely treatment should be performed. Therefore, in identifying the acquired heart defects, it is not necessary to delay with the implementation of medical recommendations.

In cardiology, there is such a term as heart failure. What threatens this pathology is important to know all patients with severe cardiovascular disease. The timely provision of medical care helps to alleviate the patient's condition with this pathology, and in some cases prevent a sudden cardiac arrest.

Спасибо за информацию!